Data Advances Improvements in Stroke Care Delivery, Reducing Mortality

- 33.8 percent relative reduction in mortality for patients who have had a stroke.
- $118K in cost savings, the result of a 23.7 percent relative decrease in average variable costs, and a 19.4 percent relative reduction in LOS for patients who have had a stroke. Patients were able to spend 39 more days at home.
Thibodaux Regional Health System had implemented evidence-based stroke care interventions in its emergency department. However, the organization was not meeting its established goals for early identification and treatment. With strong leadership support and the help of analytics, the organization’s stroke care transformation team was able to identify opportunities for improvement, culminating in improved care delivery through facility-wide automated alerts and a reduction in the need to transfer patients to other facilities for treatment.
FOR PATIENTS EXPERIENCING A STROKE, TIMELY CARE IS CRITICAL
For Americans, stroke is the leading cause of severe long-term disability, the fifth leading cause of death, and accounts for $34 billion in healthcare costs annually. When it comes to patients suffering from a stroke, early recognition and treatment improve stroke outcomes.1,2
Thibodaux Regional Health System, a nationally recognized hospital for excellence in patient care, is committed to providing high-quality, comprehensive services. Leadership turned their attention to the stroke population, hoping to identify opportunities to improve early recognition and treatment.
INCOMPLETE DATA SLOWS IMPROVEMENT OF STROKE OUTCOMES
Despite having implemented evidence-based stroke care in the ED, Thibodaux Regional was not meeting organizational goals for early stroke identification and timely intervention. The hospital lacked a standardized process for early identification of patients with a stroke. When stroke was identified, there was not a standard mechanism to notify providers, which delayed diagnostic testing and treatment. Additionally, when it came to judging performance on timely interventions, Thibodaux Regional lacked actionable data. It needed a comprehensive data-driven approach for early notification of possible stroke, including improved door-to-evaluation and treatment goals to reduce mortality, minimize transfers, and provide quality patient care.
Another problem was the lack of complete data on certain patients. Thibodaux Regional lacked continuous neurology coverage, which necessitated a higher-than-desired volume of patients being transferred to other acute-care facilities for treatment. The transfers represented lost opportunities to provide care across the continuum and impacted patient satisfaction.
CARE TRANSFORMATION TEAM DRIVES DATA-DRIVEN IMPROVEMENTS
With the support of the chief executive officer and senior executive leadership, Thibodaux Regional established a stroke care transformation team—an interdisciplinary team including the medical director, vice-president of nursing, ED director, intensive care staff, quality improvement experts, unit coordinators, nurse educators, and frontline nursing staff—to develop and implement a stroke care improvement plan.
Thibodaux Regional utilized the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications, including the Stroke Analytics Accelerator to monitor and analyze stroke care, reduce stroke-related costs, and improve clinical outcomes. Using data from the data platform, Thibodaux Regional identified the variability of stroke care processes impacting mortality rates and intervention times, as well as the conditions that led to patients being transferred to other facilities.
Using this data, the stroke transformation team prioritized efforts to reduce door-to-CT scan time as part of the overarching goal of reducing the door-to-needle time (DTN) for patients admitted through ED triage. After reviewing best practices and participating in the accelerated practices program at Health Catalyst University™, the stroke team focused its efforts on engaging frontline staff, along with nursing and physician leaders, in improving stroke recognition, minimizing time to interventions, and providing the highest quality of care possible for the community.
Emergency department providers, nurses, and technicians took ownership of the work to improve the quality and timeliness of stroke care. Thibodaux Regional provided its interdisciplinary team education to improve early recognition of signs and symptoms of stroke, to recognize uncommon symptoms, and to identify the high acuity patient needing immediate transfer to higher-level care.
Thibodaux Regional incorporated process changes beginning in ED triage to improve stroke care. It implemented a stroke assessment scale and order set, standardized stroke team notifications, utilized protocol for tissue plasminogen activator (tPA) administration, and incorporated unique visual identifiers for patients with stroke to improve early recognition and reduce intervention times, including:
- Door-to-triage stroke alert.
- Door-to-provider evaluation.
- Door-to-lab results.
- Door-to-CT completed with results.
- Door-to-tPA administration.
The process changes, notifications, order sets, and algorithms to prioritize care were optimized to align with the ED triage registered nurse (RN) and provider workflows, ensuring priority interventions were completed within the first hour of stroke identification. When a stroke is suspected, the ED triage RN activates stroke alert sending an electronic notification to the ED provider, radiology, lab, and pharmacy departments. Stroke alerts are aimed at getting the stroke team to the bedside of the patient more quickly while simultaneously triggering diagnostic testing and potential medication needs. Automated alerts update radiology, lab, and pharmacy of patient status every three minutes, ensuring their readiness.
To reduce patient transfers, Thibodaux Regional now has a neurologist on staff. Staffing adjustments in radiology along with visual identifiers, ensure prioritization of CTs for patients with stroke, and timely communication of results directly from the radiologist to the ED provider. Additionally, Thibodaux Regional moved tPA from the pharmacy to the emergency department trauma cells, eliminating the time needed for pharmacist notification and medication preparation.
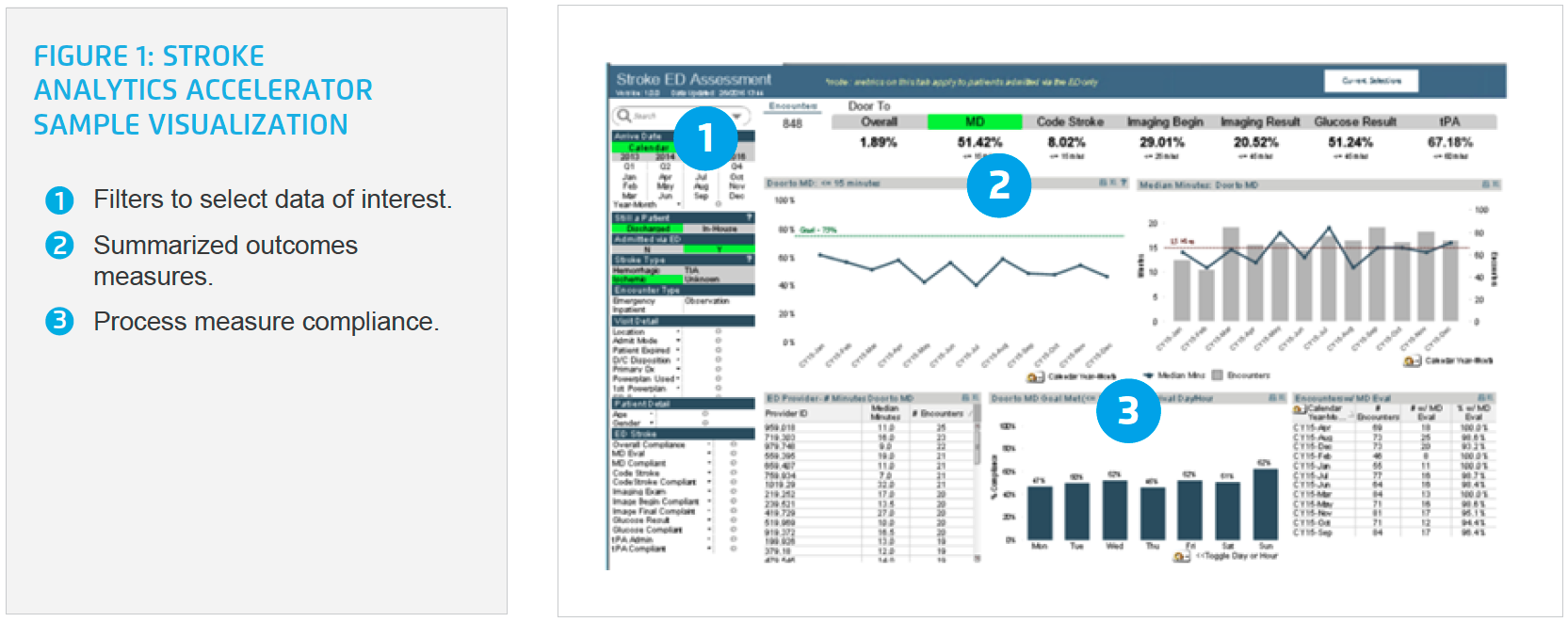
The organization leverages the analytics accelerator to monitor performance for process measures impacting stroke care such as door-to-provider evaluation, door-to-CT, and door-to-needle times. Using the analytics accelerator, Thibodaux Regional can quickly and effectively monitor the timeliness of interventions affecting mortality and transfer rates for patients with stroke (see Figure 1).
The ED stroke team uses data from the analytics accelerator to drive unified care, using data to identify successes and recognize areas for improvement. The stroke team, executive leadership, and care transformation teams use data from the analytics accelerator to monitor performance, providing feedback to physicians and nursing staff, ensuring everyone sees the direct link between intervention changes and patient outcomes.
RESULTS
Thibodaux Regional’s data-driven stroke improvement efforts have improved the consistency and timeliness of care provided to its patients, positively impacting clinical, operational, and financial outcomes.
- 33.8 percent relative reduction in mortality for patients who have had a stroke.
- $118K in cost savings, the result of a 23.7 percent relative decrease in average variable costs, and a 19.4 percent relative reduction in LOS for patients who have had a stroke.
- Patients were able to spend 39 more days at home.
- 48 percent relative decrease in door to needle time and a 21 percent relative reduction in door to CT performed time.
- Half as many patients transferred to another acute care facility since stroke improvement plan implementation.
- 25.3 percent relative increase in patient satisfaction scores, with current ranking at the 99th percentile.
“It is powerful to give staff the meaningful data they need to manage process and metrics daily—we can see a problem immediately instead of waiting days to obtain the data.”
– Danna Caillouet, RN, Director of Quality Improvement
WHAT’S NEXT
Thibodaux Regional plans to expand stroke improvement efforts to the inpatient setting, designating a stroke response team and order sets aimed at standardizing care. Leadership will continue to provide community education to prevent the incidence of stroke and help ensure timely recognition and treatment.
REFERENCES
- Centers for Disease Control and Prevention. (2019). Stroke facts.
- Harvard Medical School. (2017). Recognizing stroke early.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.