Data-Driven Care Transformation Continues to Reduce Deaths from Sepsis

- 36.4 percent relative reduction in sepsis mortality rate, sustaining previous improvement for more than three years.
- 1.6-day reduction in ICU length of stay (LOS) for patients with sepsis.
- 1.1-day reduction in inpatient LOS for patients admitted to the hospital for sepsis.
Thibodaux Regional Health System had improved sepsis mortality rates, yet it recognized the challenges associated with sustaining and further improving care outcomes. Driven by a mission of patient-centered excellence that starts with the chief executive officer, the Board, and leadership, Thibodaux Regional’s sepsis care transformation team utilized its data platform and analytics applications to help facilitate data-driven, sustained improvements.
IMPACT OF SEPSIS MORTALITY
Sepsis impacts a minimum of 1.7 million adults in the U.S. and is responsible for nearly 270,000 annual deaths. One-third of all hospital deaths are patients with sepsis.1,2
Thibodaux Regional Health System, a nationally recognized hospital for excellence in patient care, is committed to providing the highest quality, most cost-effective healthcare services possible to the people of Thibodaux and the surrounding areas. The organization worked toward sustaining sepsis improvements.
CREATING A PLAN FOR SUSTAINED SEPSIS IMPROVEMENT
Thibodaux Regional had successfully reduced its sepsis mortality rate, length of stay (LOS), and costs following the inception of its sepsis care transformation team, and the implementation of standard, evidence-based sepsis care practices. While it had lowered sepsis mortality, thereby saving lives, the hospital was aware that it needed a plan to sustain these improvements. It also had the opportunity to improve some challenging aspects of sepsis care, including compliance with three-hour and six-hour bundle elements like fluid resuscitation.
Providers had voiced concerns with initiating large volumes of fluids on patients who may be at risk of fluid volume overload. Once initial treatment following the three-hour bundle had been delivered, continued follow-up and six-hour bundle compliance showed inconsistencies, including repeating lactic acid and monitoring continued fluid resuscitation needs.
There was also confusion related to two different workgroups at Thibodaux Regional—the sepsis care transformation team and the core measures team. The two workgroups focused on the same patient population, occasionally resulting in confusion and mixed messages about expectations.
Thibodaux Regional needed a plan to ensure it could sustain the gains made in preventing patients from needlessly dying from sepsis.
DATA-DRIVEN APPROACH GUIDES SEPSIS CARE TEAM EFFORTS
Clinical improvement at Thibodaux Regional starts at the organization’s top, with strong support from CEO Greg Stock and the Thibodaux Regional executive team. Executives, including Stock, serve on the care transformation steering team, which is responsible for oversight of the hospital’s clinical improvement efforts.
Senior leadership has continued to champion the sepsis care transformation team, which has adjusted its membership and priorities as improvement needs have grown and changed, including the focus shift from the emergency department (ED) to the intensive care unit (ICU). Initially concentrated on improving early recognition and treatment of sepsis within the ED, active participation of physicians in this department was required. As the group’s focus changed to improving sepsis care in the ICU, less time was required of ED physicians, and the team requested more time from its critical care physicians.
To minimize confusion resulting from sepsis care transformation team goals compared with core measure requirements and communication coming from two different groups, the sepsis care transformation team added the staff members responsible for core measures to the transformation team. This created consistent goals and messaging from both teams related to interventions aimed at reducing sepsis mortality and LOS, while also meeting the core measure requirements.
Analytics inform approach to sepsis care improvements
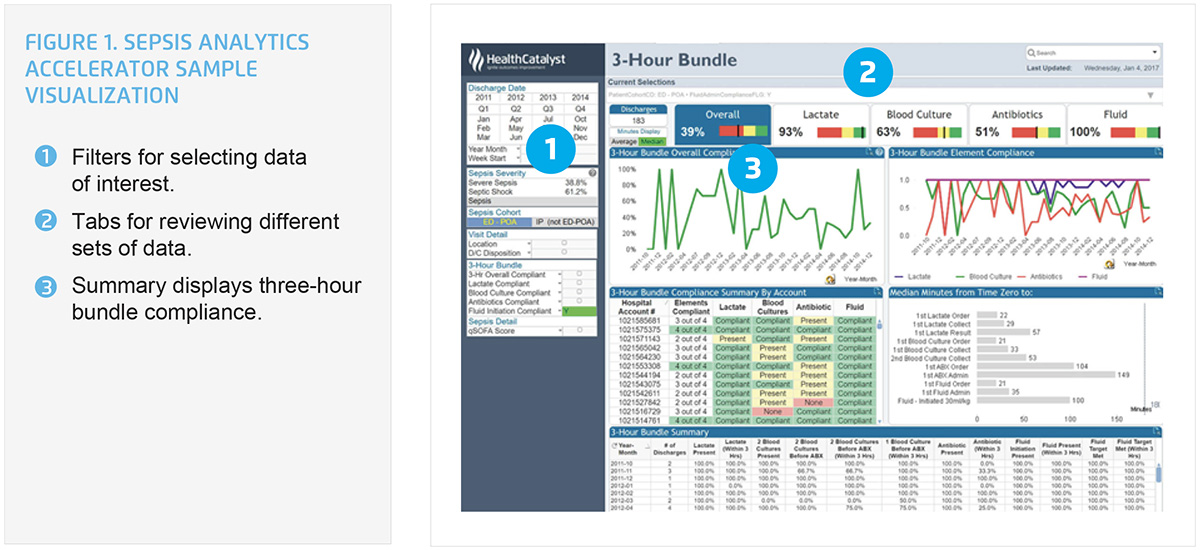
Thibodaux Regional uses the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications, including the Sepsis Analytics Accelerator, to help facilitate data-driven improvement. The analytics accelerator allows the hospital to monitor each portion of the three- and six-hour bundle, including aggregate and patient-level detail for:
- Measurement of lactate level.
- Obtaining blood cultures prior to administration of antibiotics.
- Administration of broad-spectrum antibiotics.
- Rapid administration of fluids for hypotension or a lactate level greater than four mmol/L.
- Administering vasopressors if the patient has hypotension during or after fluid resuscitation to maintain mean arterial pressure greater than 65 mm Hg.
Data transparency key to positive outcomes
Thibodaux Regional uses the analytics accelerator to ensure it maintains its previous improvements, monitoring the timely identification and treatment of sepsis. The hospital’s sepsis care transformation team uses the analytics to continually inform providers and nursing care staff about their performance. Data transparency plays a significant role in sustaining and further improving positive outcomes.
Providers are informed of performance related to patient mortality and the impact of early recognition and treatment on patient outcomes. Providers in the ED receive data about their performance quarterly as well as that of their peers, and family and internal medicine providers semi-annually. Ongoing education and communication are given to ensure the care team continually “thinks sepsis.”
Thibodaux Regional continues to refine the tools used by its clinical staff to identify sepsis and has added “recent” fever, rather than only including “current” fever to its sepsis screening tool. Increasingly, the hospital’s care teams are “thinking sepsis,” monitoring patients to ensure sepsis is rapidly identified and treated.
Having evaluated its performance using the analytics accelerator, Thibodaux Regional recognized the opportunity to improve the recommended intravenous fluids ordering. The sepsis care transformation team elicited support from providers and the pharmacy, updating the sepsis order sets, thereby simplifying orders for the desired fluid volume. Revised order sets have 30 milliliters per kilogram, pre-checked to make it easier for providers to order evidence-based fluid recommendation. For patients who may be at risk of fluid overload, providers can elect to administer fluid at a slower rate.
Thibodaux Regional has also improved the timeliness of central line insertion for patients with sepsis, ensuring the ability to administer the volume of fluids required for effective fluid resuscitation.
RESULTS
Analytics and a data-driven improvement methodology have allowed Thibodaux Regional to sustain and further improve its sepsis care. The medical center has achieved a:
- 36.4 percent relative reduction in mortality rate, sustaining previous improvement for more than three years.
- 1.6-day reduction in ICU LOS for patients with sepsis.
- 1.1-day reduction in inpatient LOS for patients admitted to the hospital for sepsis.
“Through this initiative, we changed the culture among physicians to more readily and easily identify sepsis and be aware of it as a possibility in the diagnostic workup. We have a greater understanding of sepsis and can better treat patients.”
– David Patten, MD, Pulmonologist/Critical Care Specialist
WHAT’S NEXT
Thibodaux Regional’s sepsis care transformation team is continuing to find ways to reduce sepsis mortality. Every meeting, the team identifies an opportunity to improve a process and plans to continue enhancing its six-hour bundle compliance.
REFERENCES
- Centers for Disease Control and Prevention. (2016). Sepsis – Data & Reports.
- Centers for Disease Control and Prevention. (2016). Making health care safer – Think sepsis. Time matters.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.