Analytics Improves Insight into PMPM, Reduces Liabilities in Rate-Setting Agreements

- Timeliness of rate-setting utilization data improved from two years to just a few months.
- Identified opportunities to effectively reduce liabilities, helping to ensure ongoing financial viability of the organization.
- Rapid integration of new member cost data.
In the U.S., Medicaid provides health coverage to more than 68 million low-income men, women, and children, and is funded jointly by states and the federal government. Growing at an unsustainable rate, Medicaid programs have left many states with the challenge of finding new ways to create fiscally stable systems of care that also improve health outcomes.
Oregon established an accountable care model unique to the state composed of coordinated care organizations (CCOs) which are local organizations charged with managing care for members of the Oregon Health Plan—Oregon’s Medicaid program—in addition to finding innovative ways to meet the goals of the Triple Aim: better care, smarter spending, and healthier people.
Health Share of Oregon (Health Share) is the state’s largest CCO serving 320,000 Oregon Health Plan members in the Portland-metro region of Clackamas, Multnomah, and Washington counties. Health Share operates as a collaborative of ten managed care entities, or “plan partners,” that bear financial risk for and provide management of physical, dental, and behavioral health benefits. Like all CCOs, Health Share required accurate and timely data to support forecasting for rate-setting to remain financially solvent and limit liability in this innovative model.
A PROACTIVE APPROACH TO SUSTAINABILITY—OREGON’S COORDINATED CARE ORGANIZATIONS
Medicaid provides health coverage to more than 68 million low-income men, women, and children in the U.S., and is funded jointly by states and the federal government. The rapid growth of this program could prove unsustainable unless new models of care are created that provide fiscal stability as well as improve health outcomes.
Determined to find a sustainable way to improve the health of its population, the State of Oregon embraced the challenge of the Triple Aim: improved care and smarter spending by transforming the delivery of healthcare.1 To help achieve this goal, and consistent with its pioneering spirit, Oregon established a managed care model unique to the state in 2012. The model is composed of coordinated care organizations (CCOs) which are responsible for providing comprehensive care for low-income Oregonians including working families, children, pregnant women, single adults, and seniors, who are covered by the state Medicaid program, the Oregon Health Plan.
The Oregon Health Plan pays CCOs using a PMPM capitation payment for all covered services. The payment agreements for the CCOs include upside and downside risk for costs. While CCOs are eligible to receive additional payments for cost savings, the global budget is capped because Oregon’s federal waiver with CMS requires that Oregon contain rate increases to 3.4 percent per year or less—supporting the goal of generating $11 billion in savings over ten years.2,3
The challenge of trying to stay solvent while balancing all of these constraints and developing a unique collaborative model put a good deal of pressure on the state’s CCOs, and the implementation was rife with challenges. Health Share, the state’s largest CCO serving 320,000 Oregon Health Plan members in Clackamas, Multnomah, and Washington counties was up for the challenge.
ACCESS TO DATA AND ACCURATE FORECASTING: CRITICAL TO IMPROVING PMPM PAYMENT PERFORMANCE SUCCESS
Health Share uses a cost template provided by the Oregon Health Authority (OHA) to annually report financial costs and anticipated trends. OHA uses the cost template to establish the PMPM fee Health Share will receive. While Health Share previously used the cost template to facilitate rate-setting processes, the data available to inform the rate-setting did not always support accurate forecasting of the anticipated trends and accurate insight into emerging experience. The data used were somewhat aged, time intensive to access, and did not account for shifts in the size of the population, or changes in treatment options.
As a result, annual utilization rates for specific diagnosis-related groups—some of which are assigned to a specific risk corridor or specific benefits—did not always match well with actual usage. This resulted in millions of dollars in liabilities to either Health Share, its plan partners, or to the OHA. For example, in one rate group, the historical data suggested a PMPM utilization rate that was double the actual amount utilized, resulting in millions of dollars in downside risk and liability for Health Share to OHA.
Furthermore, it was burdensome for Health Share to track its medical loss ratio (MLR)—required reporting for both the State of Oregon and the Affordable Care Act. The MLR is a measure of the percentage of premium dollars that a health plan spends on medical claims and quality improvements versus administrative costs and is used by the government to ensure that health plans provide value to enrollees. The data needed to accurately perform this calculation resided in multiple, unrelated data sources, making it difficult and costly for Health Share to monitor, obtain, and meet reporting requirements.
ANALYTICS DELIVERS EASY ACCESS TO VITAL DATA, UNLOCKING KEY INSIGHTS
For success as a CCO, Health Share needed enhanced data and analytics that would enable it to more accurately forecast PMPM utilization rates, facilitate accurate rate-setting agreements, and minimize liabilities, thus improving PMPM performance success. To accomplish this, Health Share implemented the Health Catalyst® Analytics Platform and broad suite of analytics applications, including PMPM Analyzer. The PMPM Analyzer supports a holistic evaluation of the drivers of PMPM payment performance (see Figure 1). This claims-based tool gives an in- and out-of-network view of payment trends and gives Health Share the power to understand how its providers, members, and specialty areas are contributing to overall PMPM payment performance.
With easy access to drillable and detailed information, Health Share can investigate trends and theories leading to better informed and superior strategies to provide more Oregonians with better service at a lower cost.
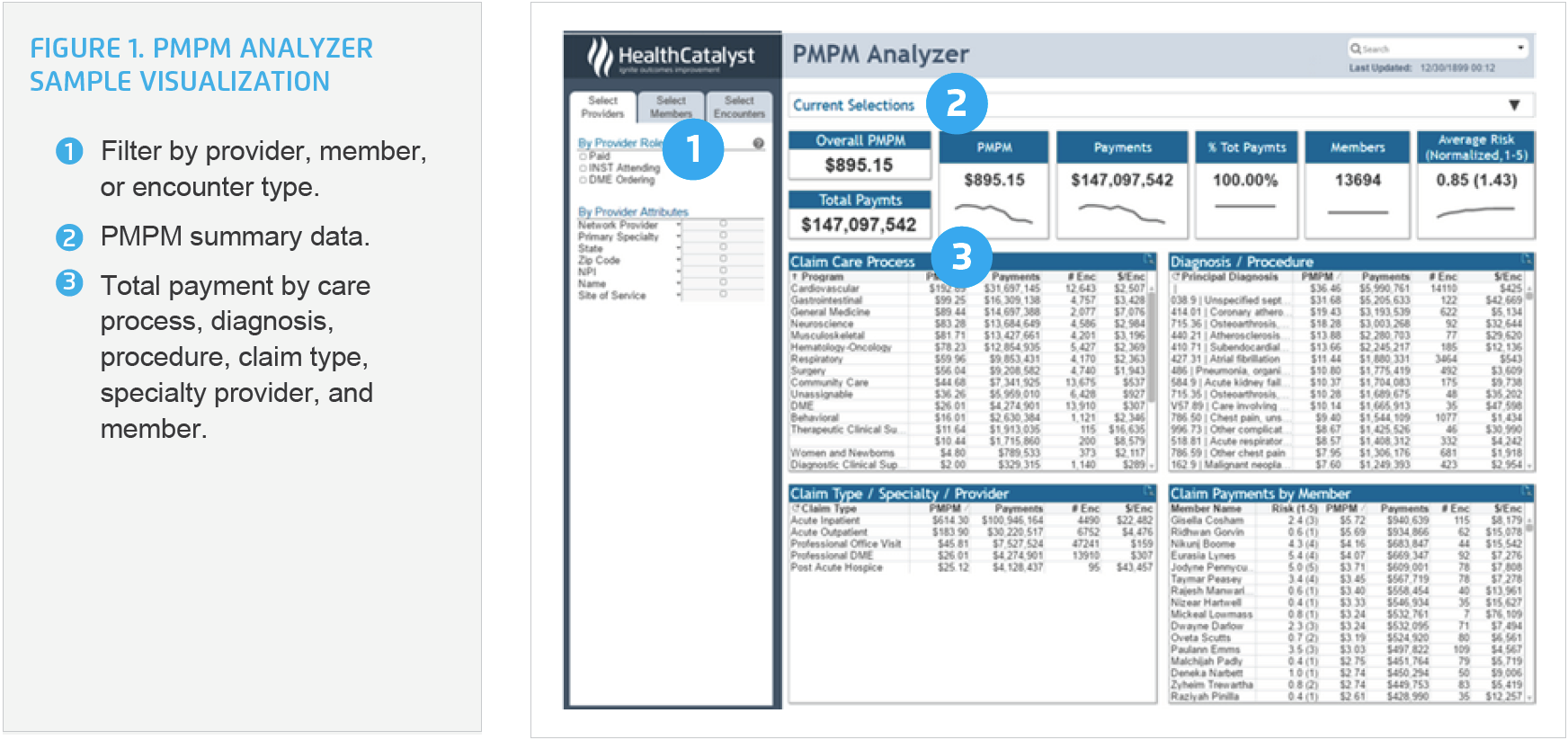
To better understand the needs of specific populations, Health Share can use the application to visualize its performance for an entire book of business and can easily drill into the data to identify total spend by care process, diagnosis, claim types, or member. This ready access to data has allowed Health Share to monitor performance and proactively manage liabilities. Rather than relying on manually developed reports using dated information, Health Share is now able to quickly create and save custom views within the analytics application, providing ready access to PMPM data for the areas of spend it needs to meticulously monitor. Health Share can easily identify areas of both under-spending and over-spending and is able to correct its performance in a timely manner to prevent liabilities.
In one notable example, Health Share was able to visualize data from the analytics application for one of its risk corridors—a risk-sharing mechanism in which Health Share and OHA share in both higher and lower expenses outside of the target amount. Health Share used the analytics application to identify that the historical rates used to establish the risk corridor payment were significantly higher (due to changing drug prices) than the current spend rate. Health Share used mid-year data from the analytics application to reflect more accurate emerging trends and negotiate a reduced rate of payment—decreasing liability and the need to pay dollars back to OHA at the end of the year.
When Health Share was faced with a sizeable increase in members, it was able to easily flag the new members in the analytics application, enabling accurate tracking of new expenditures for the new members, better informing future rate-setting agreements.
Another win for Health Share is the ability to use the analytics application to easily monitor and report MLR. Reporting this ratio is required at the state and national level and was difficult for Health Share to do before it had an analytics solution. The analytics application includes a visualization of Health Share’s allowed and paid MLR. Health Share uses the analytics application to monitor and report the MLR by rate group, plan type, and plan partner, providing them with improved, expanded, and accurate information.
RESULTS
Analytics has improved and expanded Health Share’s visibility into all aspects of PMPM expenses, enhanced the timeliness and accuracy of available data, and supported Health Share in proactively managing its downside risk and associated liabilities. Health Share has achieved meaningful results that have positively impacted program viability and success:
- Timeliness of rate-setting utilization data and emerging experience improved from two years to just a few months.
- Identified opportunities to effectively reduce liabilities, helping to ensure ongoing financial viability of the organization.
- Rapid integration of new member cost data.
- 170 hours of analyst time saved each year when completing quarterly regulatory reports, including accurate MLR reporting.
“For success as a CCO, Health Share needed enhanced data and analytics that would enable it to more accurately forecast PMPM utilization rates, facilitate accurate rate-setting agreements, and minimize liabilities, thus improving PMPM performance success.”
WHAT’S NEXT
Health Share plans to continue to use PMPM to monitor expenses and meet regulatory reporting requirements. In addition, Health Share will continue to evaluate PMPM to identify opportunities to further reduce the cost of healthcare in Oregon.
REFERENCES
- Oregon Health Authority. (2012). Coordinated care organizations – Implementation proposal.
- McConnell, K. J. (2016). Oregon’s Medicaid Coordinated Care Organizations. JAMA, 315(9), 869–870.
- Kliff, S. (2013). Can Oregon save American health care? The Washington Post.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.