How to Improve Appendectomy Care Outcomes Using Advanced Analytics in Healthcare

Establishing a single source of truth through the EDW has given us a shared understanding of appendicitis outcomes across the enterprise. Seeing what is possible with data is driving significant cultural transformation in our organization — and moving us into a new era of measurement.”
– Kathleen E. Carberry, RN,
MPH Director of Hospital Outcomes and Impact Service
- Developed appendectomy population health analytics platform
- Improved patient outcomes and reduced costs through cultural transformation
Approximately 250,000 cases of appendicitis occur every year in the United States. In fact, appendicitis is the most common acute surgical condition of the abdomen.1 These cases account for an estimated one million hospital days per year and consume 11.8 percent of all hospital discharges for gastrointestinal diseases.2
Research has shown that the mean length of stay (LOS) for appendectomy procedures can vary significantly based on a number of factors, including severity of appendicitis (e.g., simple, complex), operating room availability, surgeon preferences, nursing policies and hospital systems.3 Thus, ample opportunities to improve appendectomy care outcomes by streamlining processes and implementing evidence-based practices exist. Appendectomy care became an important focus for Texas Children’s Hospital, a not-for-profit organization consistently ranked among the top children’s hospitals in the nation, based on the large volume of appendicitis patients and the variation in practice. They also wanted to address the higher costs and increased morbidity related to severe (complex) appendicitis patients.
Texas Children’s has long recognized the importance of using technology to enable the delivery of higher-quality and lower-cost patient care. Quality and efficiency have become even more important to the hospital amid the impending transformation of the reimbursement system from fee-for- service to value-based payments. The hospital system is moving from cost-based reimbursement for Medicaid to a form of value-based payment under which hospitals that improve efficiency can keep the savings.
This case study details how Texas Children’s is using analytics technology, team-based processes and evidence-based best practices to drive higher- quality, lower-cost care for appendicitis.
THE PROBLEM: LACK OF DATA, LACK OF BUY-IN
Consistent with nationwide trends, Texas Children’s found that appendectomies represented one of their largest categories of surgical cases — with more than 1,000 appendectomy procedures each year. Based on the incomplete data they had gathered, they also discovered tremendous variability in LOS, costs and outcomes.
To improve costs and outcomes, the quality improvement team worked with the hospital’s Evidence Based Outcomes Center (EBOC), which develops evidence-based clinical guidelines to help clinicians manage the complexity of care and minimize variations in clinical practice. The team identified evidence-based practice guidelines and rolled them out among clinicians; however, there was no system in place to monitor outcomes after implementation of the guideline, or to track clinician adherence to the guidelines over time.
Another challenge Texas Children’s faced in improving appendectomy care was a lack of data. What data they had was delayed and retrospective and wasn’t gathered in a uniform, systematic way. The typical method for gathering the necessary data was for research residents and fellows to pull data from charts and analyze results. This effort was important in terms of generating answers to research hypotheses, but was not flexible or efficient in providing near-real time outcomes data necessary for guiding patient care. Additionally, it consumed resources and required retraining as residents completed their research rotations.
APPLYING THE THREE SYSTEMS APPROACH TO APPENDECTOMY PROCEDURES
Texas Children’s turned to a technology-driven approach to enable its clinicians to deliver higher-quality and lower-cost appendectomy care. The hospital had already worked with Health Catalyst to implement a clinical, analytic and process-based framework for value-based transformation. This framework, known as the Three Systems Approach:
- Improves measurement and analytics (an analytics system)
- Creates permanent cross-functional workgroup teams focused on identifying, deploying and monitoring the effectiveness of quality improvements (a deployment system)
- Deploys a data-driven approach to implementing evidence-based best practices (a content system)
The hospital was using this framework to improve other clinical and operational processes, such as asthma care. They determined to apply these three systems to appendectomy care. Specifically, the program incorporated the following elements:
- The Health Catalyst Enterprise Data Warehouse (EDW) platform, designed to handle the massive quantities of data in large healthcare organizations. The EDW organizes the hospital’s data into a single source of truth that serves as a foundation for data- driven improvement. The data warehouse enabled Texas Children’s to eliminate the manual data gathering process and automate data distribution. Analysts could then devote their time to discovering patterns in the data that could be used to understand where changes needed to be made.
- Population Analytics Advanced Application – Appendectomy Module, which enables teams to actively measure the effectiveness and outcomes of care improvement interventions for the specific patient population. Using an Agile development process that involved an integrated workgroup of clinicians and technical personnel, Texas Children’s was able to quickly define and refine its patient populations — and achieve buy-in from clinicians of the analytics platform as a single source of truth.
- Permanent, integrated workgroup teams that identify areas for care improvement and build evidence-based practices into the care delivery workflow. The workgroup consisted of clinicians (surgeons), a research nurse, and a data specialist and data architect. The workgroup also had ad-hoc representation as needed from other groups, such as ED clinicians and finance personnel. The team worked with clinicians and staff on the frontlines of care to evaluate and develop clinician training, nursing plans and patient education materials, ensuring effective system-wide implementation of best practices. The team received support from Texas Children’s quality department including the senior vice president of quality, chief quality officers for surgery and medicine, and the chief of clinical systems integration. They also received support from the chief information officer and senior vice president for information services. The partnership between quality and information systems, at the highest levels of the organization, was critical to the successful execution of this new data-driven care delivery paradigm.
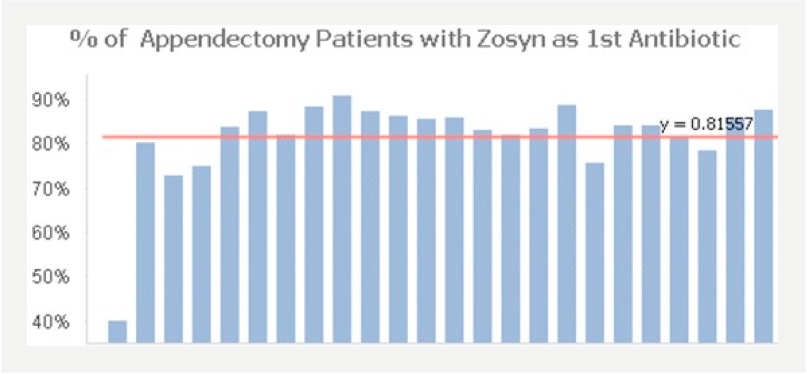
- Evidence-basedbestpractices,which guided the workgroup as it identified areas where care could be improved and standardized. To determine the points in the appendectomy care process where evidence-based best practices could be applied to standardize and improve care, the team mapped out the appendectomy procedure workflow , from diagnosis to after care. The team consulted with the EBOC to discover the latest evidence-based recommended practices. One such practice that the team incorporated into the workflow was the use of the antibiotic Piperacillin to help reduce surgical site infections by tailoring treatment to address the local microbiology of complex appendicitis.
Because the permanent workgroup owns improvement for one particular care family over the long-term and is able to work with the EDW data in near real time via easy-to-use dashboards, they are successfully standardizing excellence in their care delivery work processes.
RESULTS: PERFORMANCE IMPROVEMENT USING ANALYTICS IN HEALTHCARE
Although clinical transformation is an ongoing, iterative process, Texas Children’s appendectomy team has had impressive, measurable success in a short amount of time.
Developed appendectomy population health analytics platform
Using the EDW and the Appendectomy Module, Texas Children’s has developed a robust population health analytics platform for appendectomy care. Data from multiple source systems is now quickly integrated to enable prospective analytics in healthcare. This means that the team can assess outcomes for the population over an extended period of time and relate those outcomes to factors such as treatment protocols and suspected risk. Because clinicians were involved in developing the platform, they trust the data and use it as their single source of truth about appendectomy outcomes. Visualizations available in the Appendectomy Module allow for easy identification of improvement opportunities and quick recognition of data quality issues. It is easy for individual clinicians and analysts to delve into the data themselves without having to request a report from the IT department. These clinicians and analysts are now able to compare data across all Texas Children’s locations where appendectomies are performed and stratify data based on patient characteristics such as age, gender, type of disease, etc. Prior to the EDW and Appendectomy Module, the team would spend several months just trying to collect the data.
Improved patient outcomes and reduced costs through cultural transformation
In the Three Systems Approach that Health Catalyst advocates and Texas Children’s adopted, all systems — analytics, deployment and content — work together to establish an organization whose culture is one of data- driven improvement. The following results stem from the interaction of these three systems. Implementation of these systems results in a unique culture where clinicians on the frontlines of care use data and technology to make a difference in patients’ lives.
1. Cultural transformation
Combining a single, agreed-upon source of truth with clinician engagement enables the Texas Children’s team to use data in an ongoing cycle of continuous improvement. This effort has required concerted efforts to educate clinicians. Here is just one example of how engaging clinicians with data is driving cultural transformation. Surgeons are trained to document the severity of the case in the operative note. The team leverages an appendectomy visualization (sample shown in Figure 1) to estimate the number of severity changes that are made, which helps identify potential gaps in documentation.
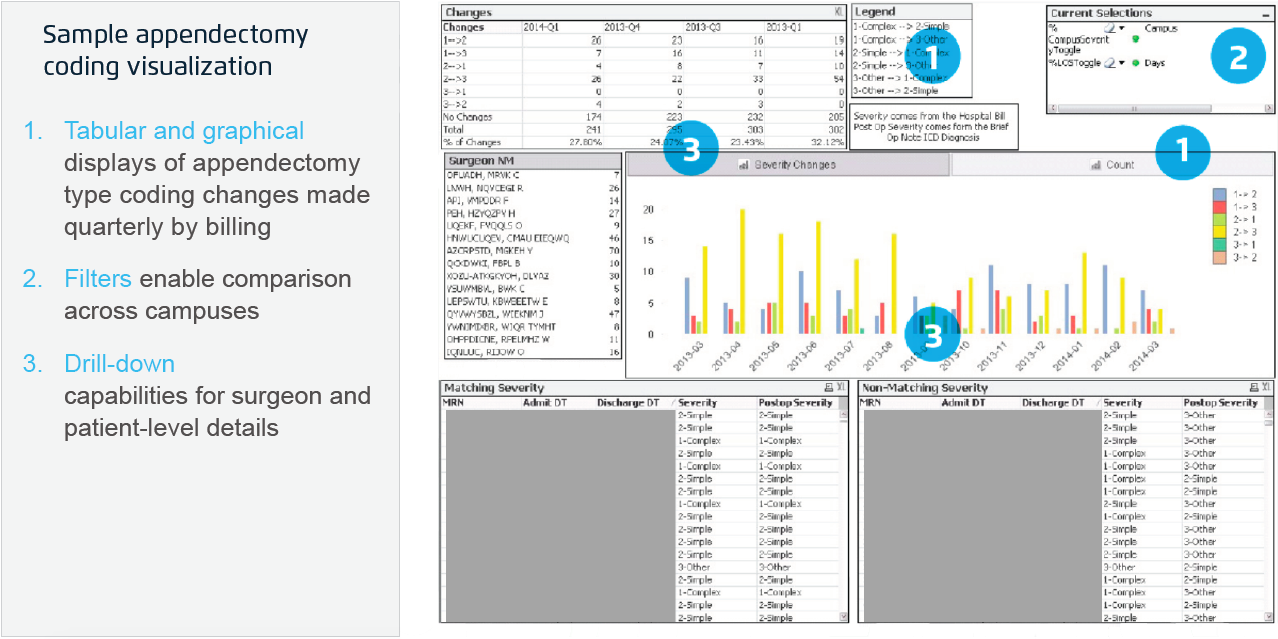
As part of education and process improvement, the team trained the physicians on the operative note template. They share the metrics with physicians to establish an ongoing culture of transformation using data. Cultural transformation efforts have also involved nurse and family education.
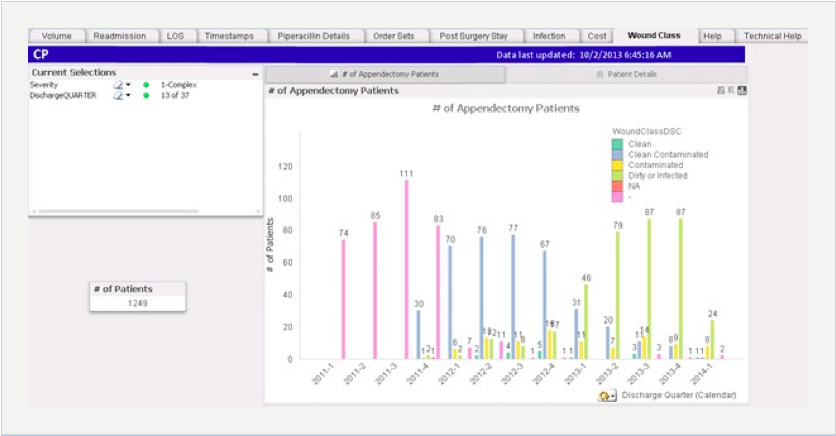
- Nursing education and engagement: The team worked with nurses on a wound classification initiative that was designed to help educate nurses on how to accurately code wound class for simple and complex appendicitis. Surgical wound class is an important and useful quality measure for risk stratification. This information is reportable to the public and third party payers, and may be linked to reimbursement for treatment of surgical site infections. The impact of training on surgical wound classifications is illustrated in Figure 2 and has resulted in the following positive year over year outcomes4:
- Increased the wound class coding by nine percent
- Increased the accuracy of the coding as demonstrated by the fact that “clean” wound classifications decreased by five percent, while “contaminated” and “dirty or infected” classifications increased by 30 and 29 percent, respectively.
- Families and patients: The team developed an education pamphlet — for simple appendicitis — to help set expectations for parents or designated caregivers of patients at the beginning of the process. This education continues throughout the care process.
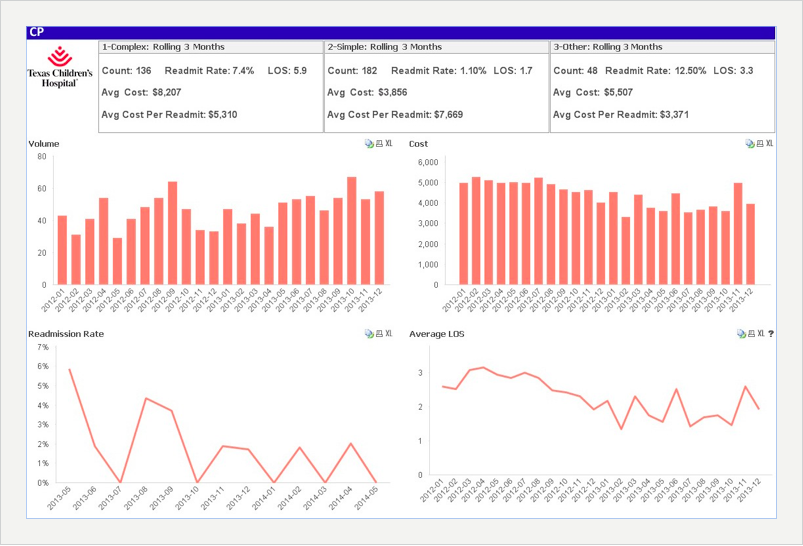
2. Improved patient outcomes and reduced costs
Using evidence-based interventions and education, Texas Children’s has successfully improved outcomes from appendectomy surgeries while reducing costs. By creating standardized processes that follow evidence- based guidelines — and ensuring the adoption of these protocols across the enterprise — the hospital has realized the following positive year over year outcomes4:
- Reduced simple appendectomy postoperative length of stay by 36 percent
- Reduced average variable direct costs by for simple appendectomies by 19 percent
- Increased postoperative simple order set adoption rates by 36 percent and postoperative complex order set adoption rates by nine percent
- Increased percentage of patients receiving recommended antibiotic (Piperacillin) as first antibiotic by 53 percent.
The following are sample visualizations from the Appendectomy Module. The team uses these graphs and other visualizations to assess its quality and cost progress.
3. End-to-end workflow optimization
The team has mapped out workflow processes and is examining the amount of time required to perform each portion of the workflow: hours from presentation to diagnosis, diagnosis to surgery and surgery to discharge. Detailed data about workflow has enabled the team to understand differences in patient flow at their two campuses. Based on data, the surgical team worked with radiology to develop a standardized ultrasound reporting template that facilitated communication among providers ultimately reducing the time interval from diagnosis to surgery and leading to prompt disposition from the emergency department. They have also used seasonality data to help predict staffing during peak times. Through these efforts, they have decreased the time from presentation to diagnosis for simple appendicitis by two percent and decreased the time from diagnosis to surgery by 19 percent for the same types of cases.
WHAT’S NEXT
The appendectomy team continues to identify opportunities to drive ongoing improvement and reduction in costs. And although Texas Children’s is using the Three Systems Approach to improve several clinical work processes throughout the enterprise, appendectomy is the first surgical procedure they have addressed. They plan to extend the methodology they have established to other surgical procedures. As its storage of data about surgical performance grows, Texas Children’s plans to establish an unprecedented level of transparency with its community. The team hopes to post clinical outcomes — including complication rates — to its website so that families and patients can see what kind of outcomes to expect from the hospital. They also plan to train clinicians to use data to counsel patients and families as they face medical decision making dilemmas. One way Texas Children’s is doing this is through “outcome rounds” at the bedside with patients, nursing, surgeons and administration. Outcomes data are used during rounds to help answer questions from family members about their child’s clinical progress.
REFERENCES
- A Mohamed, N Bhat. Acute Appendicitis Dilemma of Diagnosis and Management. The Internet Journal of Surgery. 2009 Volume 23 Number 2.
- “Appendicitis–a study of incidence, death rates and consumption of hospital resources.” PubMed Central.
- “Acute uncomplicated appendicitis: case time of day influences hospital length of stay” PubMed.
- These improvements are for calendar year 2012-2013.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.