Improving Accuracy of Clinical Documentation Positively Impacts Risk Adjustment Factor and HCC Coding

- 10 percent increase in RAF for the target population in one year.
- 72 percent relative improvement in four key problem list diagnoses.
The Hierarchical Condition Category (HCC) risk adjustment model is used by CMS to estimate predicted costs for Medicare beneficiaries, and the results directly impact the reimbursement healthcare organizations receive for patients enrolled in a Medicare Advantage plan. CMS requires that all qualifying conditions be identified each year by provider organizations. Documentation that is linked to a non-specific diagnosis, as well as incomplete documentation, negatively affects reimbursement.
Allina Health, a not-for-profit integrated healthcare delivery system serving Minnesota and western Wisconsin, needed to improve its HCC coding and clinical documentation in order to ensure the correct risk adjustment factor (RAF) was applied to its patients, since failing to do so would jeopardize its reimbursement and result in lower-than-expected compensation. After identifying opportunities for improvement by comparing its HCC risk adjustment coding data to other organizations and vendor metrics, Allina Health improved clinical documentation precision, medical diagnoses accuracy, and ensured eligible patients are seen each calendar year.
ACCURATE HCC CODING NECESSARY FOR PROPER REIMBURSEMENT
Hierarchical Condition Category (HCC) is a risk adjustment model implemented by the CMS in 2004, used to predict costs for Medicare beneficiaries based on disease and demographic risk factors.1 The HCC risk adjustment model assigns a risk score, called the Risk Adjustment Factor (RAF), to each patient as a relative measure of the probable costs of care for the individual patient. The RAF score is used to adjust capitation payments for beneficiaries enrolled in Medicare Advantage plans and some demonstration projects.2,3
The number and share of beneficiaries enrolled in Medicare Advantage has steadily climbed in the past decade. Presently, one-in-three Medicare beneficiaries is enrolled in a Medicare Advantage plan, making accurate HCC coding necessary to receive the appropriate compensation.4 CMS requires that a qualified healthcare provider identify all conditions that fall within an HCC at least once each calendar year. Incorrect documentation and non-specific diagnoses can negatively affect reimbursement for the present and future care of a patient, which could also negatively impact patient care outcomes.
Allina Health, a not-for-profit healthcare system, provides care for patients from birth to end-of-life through its 65 clinics, 49 rehabilitation locations, 23 hospital-based clinics, 12 hospitals, 15 pharmacies, and two ambulatory care centers. Accurate HCC risk adjustment coding at Allina Health is necessary for proper reimbursement and ensure positive outcomes for patients enrolled in a Medicare Advantage plan.
HCC RISK ADJUSTMENT REIMBURSEMENT LINKED TO ACCURATE, SPECIFIC DOCUMENTATION
To be successful in risk-based contracts, healthcare organizations must ensure clinical documentation accurately reflects the clinical needs and diagnoses of patients. All documentation must have the required specificity for patient assignment to a correct RAF score, and for a provider to receive appropriate reimbursement.
Allina Health’s HCC coding for CMS risk adjustment is historically lower than the national and regional averages for the Medicare ACO cohorts. Its patient population is not significantly less complex than the national population. As such, Allina Health’s HCC coding should be comparable to the average in its geographic region.
Allina Health needed to ensure its patients were correctly risk adjusted through accurate clinical documentation and HCC coding. Failure to properly assign risk to patients would jeopardize reimbursement, potentially resulting in unfair compensation for the care provided. Improper reimbursement could also limit Allina Health’s ability to reinvest in programs that provide services to patients with chronic conditions.
To ensure proper reimbursement, Allina Health needed to enable better documentation of its care for patients with chronic diseases, and it needed to ensure appropriate reimbursement for complex patient populations, so it could reinvest in patient care and infrastructure.
However, with a system of more than 60 clinics, 550 primary care providers, and little HCC specific data, it was difficult for Allina Health to determine where to focus its improvement efforts.
MORE PRECISE CLINICAL DOCUMENTATION IMPROVES HCC CODING
To better represent the complex needs of patients, Allina Health established a workgroup responsible for improving documentation and HCC coding that meets on a monthly basis. Workgroup members include nurses, physicians, coders, HCC experts, quality improvement advisors, IT, and data and analytics subject matter experts. The workgroup had HCC risk adjustment coding information from local and national conferences, other healthcare organizations, and vendors.
By comparing its HCC risk adjustment coding data against these sources, Allina Health identified opportunities for improvement. When the workgroup looked into the potential opportunities and reviewed documentation in the EMR, they found five specific, useful focus areas that Allina Health could work on quickly.
Widespread education and communication
Allina Health provided education and support to clinicians, office managers, and office staff, developing widespread understanding of the importance of accurate clinical documentation and the reimbursement impact.
Ensuring an accurate problem list
Allina Health conducted provider education on the importance of accurate documentation for the problem list, fostering an understanding among providers of some of the unique aspects of the HCC risk adjustment and coding. Besides improving coding and reimbursement, an accurate problem list also ensures that the next provider has the most accurate clinical picture of the patient.
The problem list was optimized, with the more specific common codes appearing at the top of the list presented in the EMR. Allina Health solicited provider involvement in ensuring the problem list includes only the most specific, appropriate HCC diagnosis, and that alternative, less specific, and less appropriate diagnoses are removed.
The workgroup identified several diagnoses in the EMR where a more specific HCC code was clinically appropriate for large numbers of patients and worked with providers to reduce the gap. Initial opportunities for improvement included:
- Morbid obesity (patients with a body mass index (BMI) >40), versus the less specific obesity code.
- Patients with a BMI between 35 and 40 who have an associated co-morbidity.
- Patients with type 2 diabetes who have complications: Many patient’s diagnosis indicated diabetes without complications, yet documentation elsewhere in the EMR indicated the patient did indeed have complications. Using the more specific HCC code for diabetes with complications better conveys the risk of the patient.
- Major Depression single episode unspecified: The workgroup and providers came to understand that any level of specificity provided value, whereas major depression single episode unspecified did not have a risk adjustment factor and did not accurately convey the patient’s clinical needs.
- Chronic kidney disease (CKD): Allina Health identified that a relatively large number of patients with persistently low glomerular filtration rate (the test used to determine the stage of kidney disease) did not have a diagnosis of CKD.
Ensuring patients are seen in each calendar year
Annual wellness visits are designed to address the needs and health risks of aging adults by developing or updating a prevention plan at no cost to the beneficiary. While this benefit is an effective way to engage patients and improve care, it can be difficult to identify which patients have not yet been seen during the calendar year. Allina Health developed a report that makes it easy for operational leaders to identify patients who have not yet had a visit, employing patient engagement strategies to get the patient in for their annual wellness visit.
Decision support and EMR optimization
When patients are seen, Allina Health developed decision support tools to help clinicians make new diagnoses by using the best, most specific option. Providers are reminded to address chronic conditions and document those conditions correctly. To support clinicians in selecting the appropriate HCC code, codes are identified by an “HC” after the name.
To further support these efforts, a primary care provider preference list is used to help clinicians choose specific diagnoses with a RAF value when appropriate, to satisfy ICD-10 and HCC requirements. An alert now fires for HCC diagnosis codes that have been entered in an encounter in the past three years or that are active on the problem list. The alert is silenced if the diagnosis is added to an encounter in the current calendar year or if the diagnosis code is resolved from the problem list, helping to clean up the problem lists and encourage appropriate documentation of applicable HCC codes. This also provides a more accurate representation of the patient’s complexity to the next provider of care.
Providers can use a report in the EMR to identify potential coding discrepancies, based upon discrete fields. The report identifies discrepancies for the four diagnoses that represent the greatest opportunity at Allina Health to improve outcomes, supporting care teams in taking immediate action to resolve the identified discrepancy.
- Morbid obesity: the care team adds morbid obesity to the problem list and resolves non-specific obesity codes as appropriate.
- Type 2 Diabetes with complications: providers evaluate the linkage between diabetes and other condition and add diabetes with complications to the problem list if appropriate, and then resolve historical codes.
- Major depression, single episode: providers are encouraged to specify the severity or remission status on the problem list.
- CKD: providers evaluate CKD staging, add any appropriate CKD stage, and remove old diagnoses from the problem list.
Allina Health identified that the EMR was only submitting the first four diagnosis codes, irrespective of the number of diagnoses the provider assigned. The EMR was changed and can now submit up to 12 codes per claim, with the ability to split claims to include more diagnoses if appropriate.
Trending performance using data and analytics
Allina Health developed processes, data, and analytic capabilities to track progress and provide feedback to providers and operational leaders, providing support, so patients and diagnoses are not left unaddressed during the calendar year. In addition to reports in the EMR, Allina Health leveraged its Health Catalyst® Analytics Platform and HCC Insights, an analytics accelerator designed to help health organizations improve HCC coding and more accurately reflect patient complexity.
HCC Insights can be used to identify patients who had high risk scores last year but currently do not have high scores, enabling identification of patients who may benefit from outreach, preventative care, and chronic care (see Figure 1). Allina Health can also use HCC Insights to identify chronic conditions that may not have been documented within the last calendar year and can readily identify when a more precise HCC code may be more accurate than a generic code.
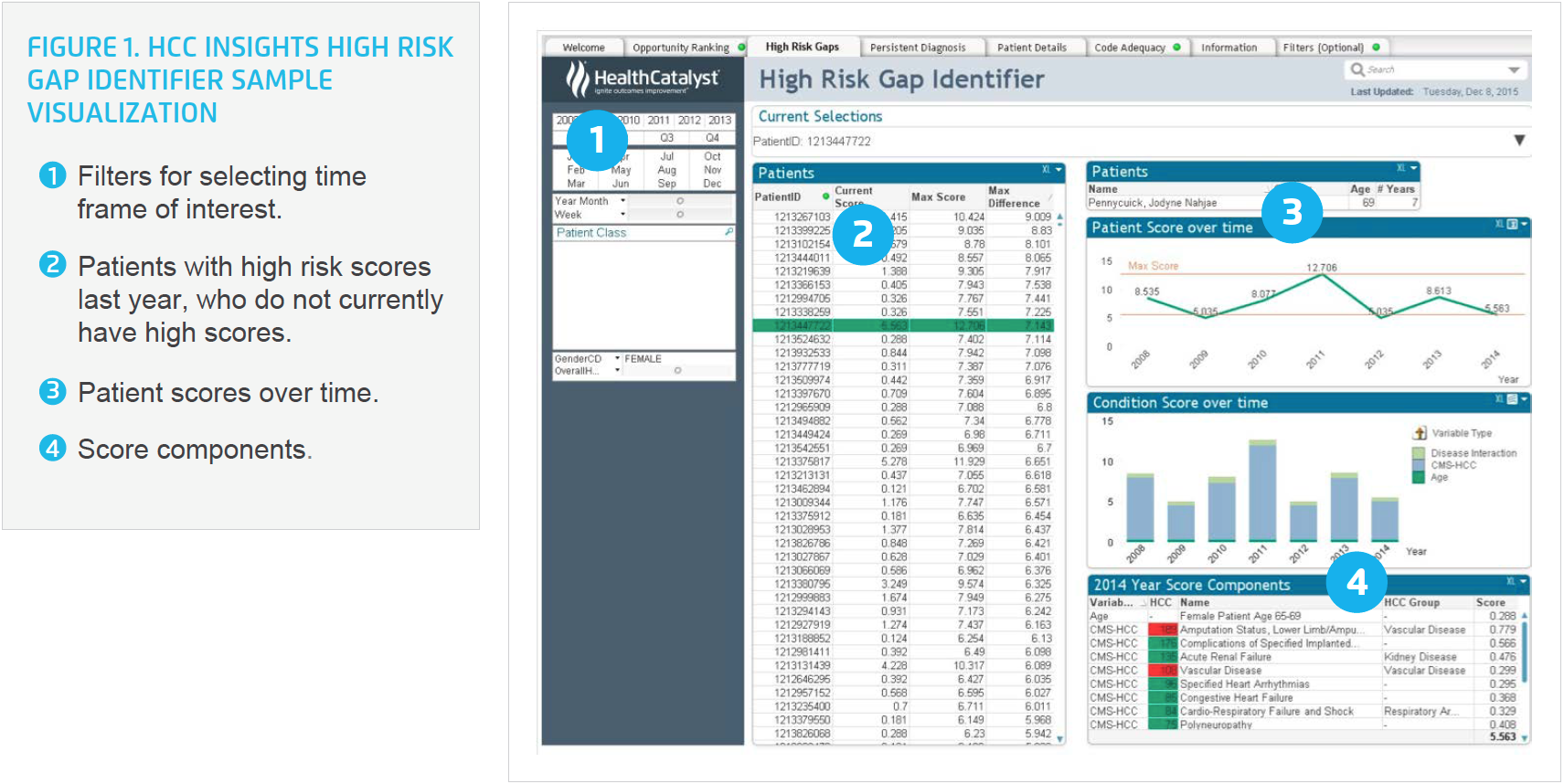
Allina Health uses the analytics accelerator to monitor coding trends, and the average RAF score at a population level to determine if additional areas of focus need to be discussed with the medical group, a hospital division, or care management.
RESULTS
By focusing on maintaining an accurate problem list, appropriate use of HCC diagnosis codes, and keeping track of annual patient visits, Allina Health can better manage the health of its patient populations and improve clinical documentation, leading to more accurate HCC risk adjustment coding. Aided by decision support, EMR optimization, data, analytics, and widespread education increasing organizational understanding about the importance of clinical documentation, Allina Health has achieved its desired improvements, including:
- 10 percent increase in RAF for the target population in one year.
- 72 percent relative improvement in problem list diagnosis in four key diagnoses (morbid obesity, type 2 diabetes with complications, major depression single episode, and CKD) in just three months.
- 13,770 potential gaps identified in September, 3,888 potential gaps identified in December, a 72 percent relative improvement.
- 10,000 diagnoses have been updated on problem lists.
“If we are documenting appropriately and thinking about the complexity of our patients, we are eligible to receive greater revenue from CMS that we can then re-invest into the infrastructure required to better meet the needs of our patient populations.”
– Nicole Kveton, RN, BSN, MHA
Vice President, Allina Health
Group Quality, Value, and Nursing
WHAT’S NEXT
Allina Health plans to continue its adaptive work to ensure appropriate documentation of HCC diagnoses. The health system has the infrastructure in place to effectively monitor and respond to changing HCC codes, changing patient populations, and changes in the health of its patient populations that may occur in the future. Allina Health sets yearly goals for HCC diagnostic resolution percentages and office visit completion rates. Progress toward the yearly goals using the HCC Insights dashboard are updated on a monthly basis and shared with clinic managers, regional medical directors, and organizational leadership. The monthly reporting on progress relative to goal allows the HCC work to remain visible for all clinics and furthers their work in documentation precision.
REFERENCES
- American Academy of Family Physicians. (n.d.). Hierarchical condition category coding – What is hierarchical condition category (HCC) coding?
- Premera Blue Cross. (2015). Medicare advantage, Risk adjustment coding.
- AAPC. (n.d.). Risk adjustment factor.
- Jacobson, G., Casillas, G., Damico, A., Neuman, T., & Gold, M.(2016). Medicare advantage 2016 spotlight: Enrollment market update. The Henry J. Kaiser Family Foundation.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.