Leveraging Risk Assessment to Decrease LOS and Cost for PCI Patients
To improve the quality of its PCI procedures and decrease costs, Allina Health recognized the need to accurately assess bleeding risk and then implemented best-practice interventions to prevent major bleeding events. Allina Health thus implemented the following interventions:
- Validation and then implementation of the NCDR bleeding risk assessment
- Education of the provider, nurse, and technician about the risk of bleeding and bleeding avoidance strategies
- Provision of real-time decision support for assessing risk for bleeding
- Increased utilization of the use of closure devices in high-risk patients
Already, physicians and patients have seen that the bleeding risk assessment tool allows clinicians to focus interventions based on risk and reduce complications. The top results from Allina Health’s interventions include:
- 5.3 percentage point reduction in (a 21.7 percent relative reduction) in complication rate.
- $1.8M cost savings.
Percutaneous Cardiac Intervention (PCI) is a minimally-invasive alternative to open heart surgery for many patients, but it is not without risks of its own. Approximately 600,000 U.S. patients will undergo PCI this year, and Allina Health is a leading provider of the procedure in Minnesota. Bleeding represents the most common non-cardiac complication of PCI and is associated with several adverse outcomes, including ischemic events, stent thrombosis, blood transfusions, increased hospital readmissions for recurrent bleeding events, and even death.
Allina Health, one of the foremost health systems in the Midwest, is a non-profit health system with 90+ clinics and 13 hospitals. Allina Health’s Cardiovascular Services include three of the highest-volume PCI centers in Minnesota. Allina Health discovered that major bleeding events following PCI procedures, though not affecting mortality, were increasing length of stay (LOS) and cost.
RISK FOR BLEEDING: A MAJOR AND COSTLY COMPLICATION
PCI, formerly known as angioplasty, is a non-surgical technique for treating obstructive coronary artery disease, including unstable angina, acute myocardial infarction (MI), and multi-vessel coronary artery disease (CAD). As the U.S. population ages, CAD is becoming more common, and PCI is the most common cardiac invasive procedure to treat patients with obstructive CAD. It is estimated that approximately 600,000 PCIs are performed annually in the United States.1
The use of anticoagulants and the invasiveness of PCI increase the risk for bleeding following the procedure. Bleeding is the most common complication of PCI2, and major bleeding events are associated with several adverse outcomes, including ischemic events, stent thrombosis, blood transfusions, increased hospital readmissions for recurrent bleeding events, and even death. Major bleeding has been associated with increased hospital costs upwards of $10,000 and increased LOS between two and six days.3
As a result of the implications of major bleeding complications, PCI providers are increasingly focused on reducing bleeding-related complications. Bleeding risk assessment prior to PCI enables physicians to selectively employ bleeding avoidance strategies (BAS) such as vascular closure devices to improve outcomes.4
Like other health systems, Allina Health is focused on avoiding PCI complications. Allina Health’s Cardiovascular Services include three of the highest volume PCI centers in Minnesota. Allina Health participates in the National Cardiovascular Data Registry (NCDR), a voluntary national quality improvement program that serves as a reporting system for in-hospital diagnostic cardiac catheterization and PCI procedures.
By developing their cardiovascular services, Allina Health is improving the quality of care, cost, and clinical outcomes for all of its cardiovascular patients. With three high-volume PCI centers as part of their organization and several serious adverse outcomes commonly associated with these procedures, Allina Health is highly motivated to look deeper into clinical variation and outcomes for patients having PCI.
INCIDENCE OF BLEEDING POST PCI INCREASES COST AND LOS
As part of its overall approach to quality improvement, Allina Health identified PCI as a potential opportunity for improvement. Looking more closely at PCI, the health system’s leaders identified substantial variation in LOS and cost across patients post PCI procedure. While clinical data and patient registries were enough to identify bleeding events retrospectively, the data did not readily identify if the bleeding event was a minor event or a major one. Financial data on LOS and cost was required to differentiate between major and minor bleeding events. Major bleeding events were the target of their PCI initiative at Allina Health, as these events provided a significant opportunity to improve outcomes and lower costs as a result of interventions.
Further review of the difference in LOS and cost revealed that post-PCI patients with the longest LOS and highest cost shared one common problem: they experienced major bleeding events after the procedure, requiring costly treatment that substantially prolonged their hospital stay. Allina Health therefore designated decreasing variability in the assessment of patient bleeding risk prior to the procedure and the purposeful employment of standard BAS, as a focus for the improvement program.
However, Allina Health faced a major roadblock to this effort: No validated, pre-procedure bleeding risk assessment tool was available. Furthermore, the health system lacked the guidelines and decision support tools that would enable effective bleeding risk assessment and management. Among the team members who provided care to PCI patients, knowledge about the risk of bleeding and effective BAS varied.
Prior to the improvement program, physicians lacked performance data and visibility into all of the risk factors for bleeding. Providers needed data on patient bleeding risk and performance/outcomes data, including provider specific data, such as their selective use of closure devices as a BAS and the outcome of the selected BAS. Cost-of-care data was also difficult to come by, as cost data was in the finance system, separate from clinical systems and not accessible to frontline providers. The separation of data in siloed systems made it difficult to identify costs associated with clinical variation or the impact of potential interventions on cost and patient outcomes.
ANALYTICS ENABLES NEW RISK ASSESSMENT STRATEGY FOR PCI PROCEDURES
In order to decrease clinical variation associated with the PCI procedure, Allina Health determined that it needed a comprehensive strategy. The strategy was architected to result in fewer complications for their high-risk PCI patients, thus improving quality while decreasing cost. Based on expert knowledge and the literature, the Allina Health team decided to focus on decreasing post-PCI bleeding through several focused interventions:
- Validation and then implementation of the NCDR bleeding risk assessment
- Education of the provider, nurse, and technician about the risk of bleeding and BAS
- Provision of real time decision support for assessing bleeding risk
- Increased utilization of closure devices in high-risk patients
The Allina Health team also realized that to be sure that these interventions were effective and sustainable, they needed a way to monitor the impact and performance of these interventions. The performance monitoring initiative started by leveraging the data in its Health Catalyst Analytics Platform, built using the Late-Binding™ Data Warehouse architecture. The data warehouse included clinical and financial data from more than 9,500 PCI cases from three separate high-volume PCI centers. Analysts worked with the data to retrospectively apply a recently developed NCDR bleeding risk assessment tool, thus conducting an analysis of the validity of the bleeding risk tool, and comparing the results with actual known financial and clinical outcomes from those cases. The retrospective study was a success, as it validated that the NCDR risk algorithm accurately stratified the patients at the highest risk for complications that lead to prolonged LOS and increased hospital costs.
The newly validated bleeding risk assessment tool proved to be foundational in making the case for change. With the tool in place, the Allina Health team prepared for implementation by educating members of the care team, including emergency department staff and physicians, interventional cardiologists, catheterization lab staff, and post-PCI providers. Educational efforts focused on the benefits of the bleeding risk assessment and bleeding risk strategies for high-risk PCI patients. The team presented education during grand rounds, in-services at various times throughout the day to align with team member’s work schedules, and in all PCI-related work areas, including the pharmacy and the lab.
Once education was completed, Allina Health integrated the NCDR bleeding risk assessment into an automated decision support tool and deployed the tool to all of the computers in the three PCI centers. Nurses in the catheterization laboratory (cath lab) were trained on the tool and instructed to complete the assessment for each patient. Once nurses entered the data into the tool, it automatically calculated bleeding risk scores and displayed, in real-time, the most current consensus BAS recommendations to all team members participating in the procedure in the cath lab.
Having validated a risk assessment tool, completed interdisciplinary education, and deployed an automated decision support tool, the team then turned its focus to improving clinical and financial outcomes by ensuring adoption of the recommended practice changes. They felt strongly that the key element that would help them drive adoption was actionable data.
The improvement effort was supported by information provided by a PCI analytics application that leveraged information in the EDW. The PCI analytics application measures the impact of provider education and the automated decision support tool on practice decisions/closure device utilization, while at the same time monitoring and evaluating complication events, cost, and quality outcomes.
Allina Health widely shared the information obtained through analytics, including information on closure device utilization by bleeding risk category, and closure device use by provider. They also shared comparative data for patients who did and did not receive a closure device, comparing LOS, cost, and complication rate. Cardiovascular Service leaders and quality improvement leaders used the analytics application most heavily, with data distributed to physicians once per week. Nurses completing the bleeding risk assessment were provided feedback and coaching regarding completion rate and consistency of screening in alignment with the NCDR bleeding risk data definitions.
The specificity of the feedback and outcomes data were the keys to gaining adoption, sustaining practice changes, and subsequently reducing complications. When physicians receive meaningful information regarding performance and the demonstrated benefits of alternate options, they will naturally change their practice.
RESULTS
Allina Health’s comprehensive strategy to better control bleeding in its PCI patients improved complication rates and cost. The impressive results shown below have come from implementation of an easy-to-use, real-time decision support tool that changed physician practice patterns, contributing to a substantial increase in closure device utilization.
With the health system’s newly standardized process, all patients are now screened for bleeding risk prior to the PCI procedure. Use of closure devices as a physician-selected bleeding avoidance strategy has nearly doubled in Allina Health’s cath labs.
To date, measurable results include:
- 5.3 percentage point reduction in (a 21.7 percent relative reduction) in complications.
As Allina Health’s preliminary research indicated, instituting measures to identify and mitigate the risk of bleeding decreased the complications experienced by PCI patients.
- $1.8M cost savings.
- 1.4 percentage point reduction (a 36.5 percent relative reduction) in LOS for patients at high risk for bleeding who receive a closure device.
Savings are a result of decreased incidence of bleeding and decreased rate of complications. Closure device utilization and cumulative cost savings are shown in Figure 1.
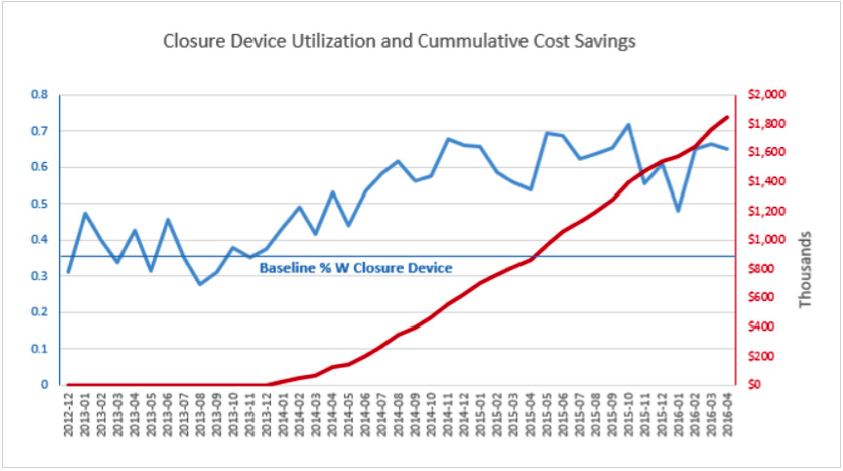
The increasing rate of closure device utilization occurred naturally. When physicians are provided data about their performance, the performance of their peers, and the data on effectiveness of closure devices, they naturally move toward the most beneficial care decision, using the closure devices when appropriate.
– Dr. Ivan Chavez
“The EDW and the analytics application give us access to a goldmine of data. We can ask one clinical question, query the data, and it opens up opportunities for improvement that we wouldn’t otherwise have known about.”
Interventional Cardiologist
WHAT’S NEXT
As a result of the initiative, Allina Health continues to improve performance and outcomes in its cath labs performing PCI. Going forward, the bleeding risk assessment tool will likely result in continued increases in the utilization of closure devices for patients at highest risk of bleeding.
Accelerating outcomes improvement is a priority for Allina Health Cardiovascular Services. Administrative and physician leadership are planning to leverage the EDW even further for the cath lab, working to identify other potentially preventable events. Upcoming projects include a plan to evaluate the incidence of contrast-induced nephropathy in the cardiac cath lab and the impact of pre-procedure hydration assessments on patient care decisions and outcomes.
REFERENCES
- Chhartriwalla, A.K., Amin, A.P., Kennedy, K.F., House, J.A., Choen, D.J., . . . Marso, S.P. (2013). Association between bleeding events and in-hospital mortality after percutaneous coronary intervention. The Journal of the American Medical Association, 309, 1022-1029. doi:10.1001/jama.2013.1556
- Go, A.S., Mozaffarian, D., Roger, V.L., Benjamin, E.J., Berry, J.D., . . . Turner, M.B. (2014). Heart Disease and Stroke Statistics—2014 Update: A report from the American Heart Association. Circulation, 129(3), e28–e292. doi.org/10.1161/01.cir.0000441139.02102.80
- Strauss, C.E., Porten B.R., Chaves, I.J., Garberich, R.F., Chambers, J.W., . . .Henry, T.D. (2014). Real-time decision support to guide percutaneous coronary intervention bleeding avoidance strategies effectively changes practice patterns. Circulation: Cardiovascular Quality and Outcomes, 7, 960-967.
- Rao, S.V., McCoy. L.A., Spertus, J.A., Krone, R.J., Singh, M., Fitzgerald, S., & Peterson, E.D. (2013). An updated bleeding model to predict the risk of post-procedure bleeding among patients undergoing percutaneous coronary intervention. Journal of the American College of Cardiology Intervention, 6(9), 897-904.
ABOUT HEALTH CATALYST
Health Catalyst is a mission-driven data warehousing, analytics, and outcomes improvement company that helps healthcare organizations of all sizes perform the clinical, financial, and operational reporting and analysis needed for population health and accountable care. Our proven enterprise data warehouse (EDW) and analytics platform helps improve quality, add efficiency and lower costs in support of more than 50 million patients for organizations ranging from the largest US health system to forward-thinking physician practices.
For more information, visit www.healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.