Integrating Data and Analytics into Provider Workflow Improves ACO Performance

- Tobacco screening and cessation plan.
- Clinical depression screening and follow-up plan
- Influenza immunization.
- High blood pressure screening and follow-up plan.
- Screening for future fall risk.
Reimbursement rates for an Accountable Care Organization (ACO) are based on the quality composite score from the Physician Quality Reporting System (PQRS) Group Practice Reporting Option (GPRO), examining best practice preventative care and primary care measures. As a result, ACO participants may receive payment adjustments based on their quality composite performance.
U.S. Medical Management (USMM), a leading provider of home-based primary care services for complex patient populations and managed care clients, also operates a multi-state Medicare Shared Savings Program (MSSP) ACO serving over 23,000 complex or fragile Medicare patients. USMM needed to support its providers in meeting their patients’ necessities, while also ensuring they were providing and documenting appropriate best practice preventative and primary care ACO measures.
USMM turned to its analytics platform and analytics applications, implementing the Community Care Advanced Application to aid its efforts. The analytics platform integrates data from the organization’s EMR, billing system, and external claims data, bringing cross organizational data into focus and delivering specific, actionable interventions needed to improve performance.
After implementing Community Care, USMM achieved a 90th percentile performance for:
- Tobacco screening and cessation plan.
- Clinical depression screening and follow-up plan.
The organization also earned an 80th percentile performance for:
- Influenza immunization.
- High blood pressure screening and follow-up plan.
- Screening for future fall risk.
ESTABLISHING ACCOUNTABLE CARE
MSSP ACO participants are subject to a number of Medicare quality reporting requirements and performance initiatives, including PQRS. The ACO’s quality composite score is based on the performance of PQRS GPRO best practice preventative care and primary care measures. As a result, ACO participants may receive as high as a four percent upward or downward payment adjustment based on their quality composite performance.1
Primary care serves as the foundation of a successful ACO, using transparent performance measures to achieve the Quadruple Aim of improving population health, patients’ experience of care, and the work life of health care providers, while reducing the total cost of care.2
USMM is a leading provider of home-based primary care services for complex or fragile patient populations as well as managed care clients. USMM operates Visiting Physician Association (VPA) practices in 14 states, constituting more than 200 primary care provider group, delivering continuity-based primary care under an integrated, physician-driven model, which includes ancillary services such as laboratory, radiology, and ultrasound-based diagnostics. The continuum also includes specialized home care, hospice, and durable medical equipment providers.
USMM provides enhanced access to health services and quality of life by removing barriers to receiving care. The integrated care model helps patients live independently longer, improves quality, promotes patient engagement, enhances medical outcomes, and reduces costs. USMM also operates a multi-state MSSP ACO serving over 23,000 complex or fragile Medicare patients and is a major participant in the Independence at Home (IAH) Demonstration. In fact, five of the fifteen practices participating in the IAH Demonstration are VPA practices. Together, these practices were responsible for caring for patients making up approximately 40 percent of the entire demonstration in year two.3
ADDING CLARITY TO DOCUMENTATION PROCESS
USMM had well-established home care protocols and procedures; however, aligning these cycles of monthly home visits with the various MSSP and PQRS reporting requirements for preventative care annual wellness visits or seasonal requirements, like influenza immunization, was confusing, making improvement efforts and performance monitoring difficult.
EMR documentation focused on patient needs and provider workflow, offering limited visibility into best practice preventative care and primary care measures. There was no easy way to determine which category best practice preventative and primary care measures were appropriate for the patient. A complex patient may qualify for as many as 12 measures annually, many of which are typically provided outside of the home setting. This made it difficult for providers to determine which measures should be addressed during specific home visits.
The time spent by providers to review previous interventions was a manual, time-consuming process that did not provide the necessary information at the point of care and detracted from their ability to focus on the patient. Additionally, there was a lack of widespread knowledge about how documentation impacted the measure. Few providers understood which documentation sources contributed to measure compliance.
USMM needed a solution that would support its providers in meeting their patients’ needs while also ensuring they were providing, and documenting, appropriate best practice preventative and primary care measures, which is critical for MSSP success.
ANALYTICS DRIVING IMPROVED ACO MEASURES TRACKING
To increase the number of patients receiving the appropriate best practice preventative and primary care, and to improve its MSSP performance, USMM needed better data and analytics that would enable it to understand its performance, identify gaps, and implement targeted improvement strategies. To meet these goals, USMM utilized the Health Catalyst® Analytics Platform and broad suite of analytics applications, including the Community Care Advanced Application.
Bringing together disparate data
The analytics platform integrates data from USMM’s EMR, billing system, and external claims data, gathering information into one source, and allowing the organization to develop interactive analytics applications and visualizations. This has brought cross organizational data into focus and has delivered specific, actionable interventions needed to improve performance.
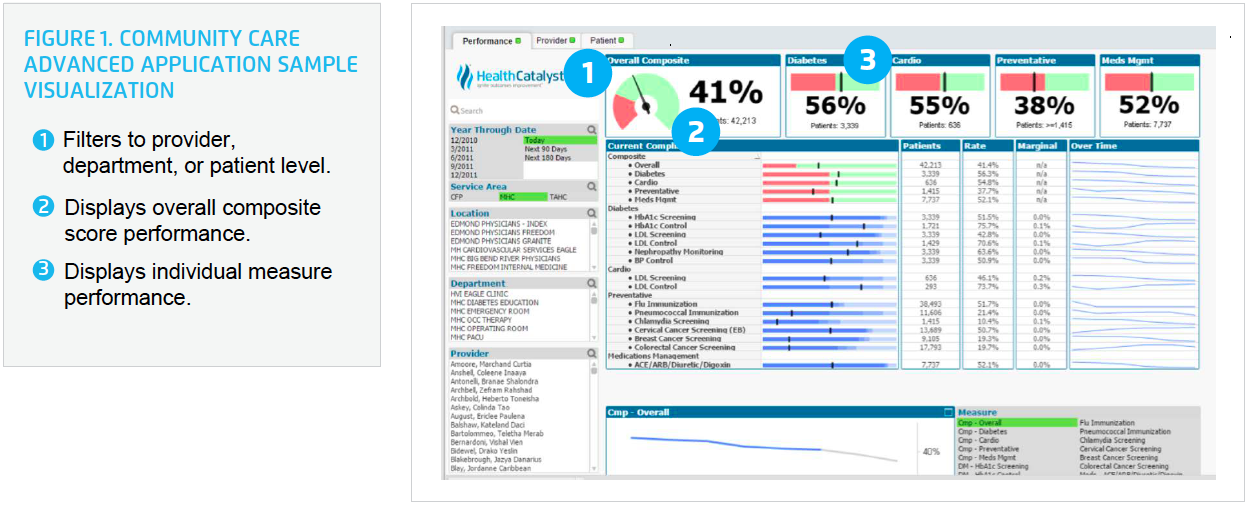
The Community Care Advanced Application focuses on providing data to help organizations review population health measures, comparing performance to national benchmarking standards for specific measures, identifying opportunities for costs savings, and visibility to track, monitor, and meet the needs of complex, high-risk patients (see Figure 1).
Supporting key ACO measures
USMM leaders, project managers, key providers, and Health Catalyst professional services conducted a deep dive into each measure to ensure data accuracy within the analytics application, including reaching out to CMS to clarify measure requirements in the unique setting of home-based primary care, clearly identifying the inclusion criteria, exclusion criteria, and denominator for each measure.
After clarifying measure requirements in relationship to home-based primary care, an iterative process was used to identify and build measures within the application, followed by beta testing to validate accuracy and usability by key end-users. Provider workflow was reviewed and standardized, ensuring consistency in documentation within the EMR and validating data integration into the application. For the first time, providers have the information required to understand the measure, documentation to meet that measure, and location of that documentation in the EMR.
To support providers in delivering the appropriate preventative and primary care, USMM integrated the provider schedule and patient-specific data into the analytics application. Practice managers and providers can now see, at a glance, the specific measures that are outstanding for the patient (see Figure 2).
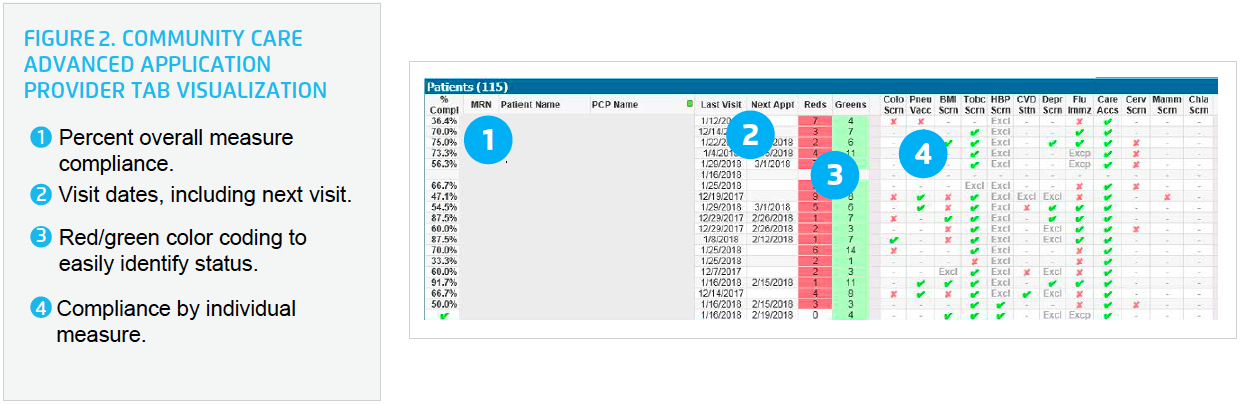
USMM trained practice managers on how to access data within the analytics application and providers on how to use information sheets on measure performance criteria, including the frequency required for each measure and population inclusion and exclusion criteria.
The data within the analytics application is used as part of the provider’s daily workflow. Using the analytics application, the practice manager populates the provider’s schedule for the day with the list of patients and outstanding best practice preventative and primary care measures for each patient that need to be addressed during home visits. Providers can then decide which care items to attend to during the visit.
Providers are able to view patient information, place orders, and document care provided at the point of care, which flows back into the analytics platform and application in near real-time. The robust information within the schedule has increased capacity for providers to identify care gaps for specific patients and take action during the current home visit.
Practice managers are able to use the analytics application to monitor and manage performance for their practice, and quality leaders can employ the data within the tool for ongoing process improvement.
RESULTS
In just eight months, USMM validated the inclusion and exclusion criteria for its patient population, successfully implementing an analytics application to assist providers in delivering the appropriate care during scheduled home visits to meet its ACO measures.
By providing home-based primary care and using real-time data integrated into the provider workflow to ensure delivery of best practice preventative and primary care, USMM has significantly improved its performance, substantially increasing the percentage of patients receiving preventative care. For the first time, the organization achieved a 90th percentile performance for:
- Tobacco screening and cessation plan.
- Clinical depression screening and follow-up plan.
USMM reached 80th percentile performance for:
- Influenza immunization.
- High blood pressure screening and follow-up plan.
- Screening for future fall risk.
USMM also achieved 80th percentile performance for the cardiology measure for heart failure: patients with left ventricular systolic dysfunction receiving either an angiotensin converting enzyme inhibitor or angiotensin receptor blocker.
USMM achieved other noteworthy improvements, including a:
- 8 percent relative improvement in diabetes HgbA1c poor control (reverse measure = lower is better).
- 25 percent relative improvement in the number of patients with diabetes receiving eye exams.
- 1.4 percent relative improvement in the documentation of current medications in the medical record.
As a result of its efforts and the high-quality of care provided to its patients, USMM has made significant contributions to Medicare savings and has been recognized as the fourth best ACO in the nation, saving over $21 million in 2016.4
“Community Care allowed us to not only build and track quality measures, but also integrate the information into the provider’s daily schedule.”
– David Vezina
Chief Information Officer
WHAT’S NEXT
USMM will continue to use this data-driven approach, hard wiring processes and moving to a proactive approach in reviewing measures, adopting updates as new information is available, and looking for additional opportunity to improve the information shared with providers, supporting them in delivering high-quality care in the patients’ homes.
REFERENCES
- Centers for Medicare & Medicaid Services. (2016). Medicare shared savings program interaction with the 2017 value modifier frequently asked questions.
- American Academy of Family Physicians. (n.d.). Accountable care organizations.
- U.S. Medical Management. (2015). U.S. Medical Management improves health,reduces costs for home bound elderly in CMS independence at home demonstration.
- Haefner, M. (2017). Top 10 MSSP ACOs in shared savings for 2016. Becker’s Hospital Review.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.