ICU Avoidance: Lowering Costs, Patient Risk, and LOS

- 636 additional ICU days made available for more critically ill patients by employing ICU avoidance strategies
- One-day reduction length of stay (LOS) for Transcatheter Aortic
- Valve Replacement (TAVR) patients
- $589,000 cumulative cost savings
A stay in the intensive care unit (ICU) is both costly and risky. In a sobering example of the latter, nearly one third of patients admitted to the ICU experience delirium, a state of cognitive impairment that can increase risk of death in the hospital. Still, many cardiovascular patients need intensive care that can only be provided safely in an intensive care unit, requiring hospitals to assure enough beds and skilled ICU staff for these patients—while quickly identifying which patients can receive care as good or better in another unit.
Allina Health has achieved this dual objective with a concerted ICU avoidance strategy for specific complex sub-populations of cardiovascular (CV) patients. The foundation of this strategy is risk-informed decisions about which patients can avoid the ICU; clinical staff education; and an analytics platform and enterprise data warehouse (EDW) from Health Catalyst that enables CV care leaders to monitor safety metrics for those patients who avoid a stay in the ICU.
WHY REDUCING ICU LOS IS IMPORTANT
The demand for CV critical care is increasing with the aging of the population and is reflected in the rising cost of critical care in general. Between 2000 and 2005, annual critical care medicine costs increased from $56.6 billion to $81.7 billion, representing 13.4 percent of hospital costs, 4.1 percent of national health expenditures, and 0.66 percent of gross domestic product. CV patients represented a significant percentage of these costs.1 Much of this care takes place in ICUs. While an integral department in all modern hospitals, ICUs are expensive to maintain, especially in an era of shrinking healthcare funding.
Further, a stay in the ICU carries real risks. One of the most sobering, nearly one third of patients admitted to the ICU experience delirium—a dangerous state of cognitive impairment. Patients with delirium are at an increased risk of dying while in the hospital, experience longer hospital stays, and have an increased rate of cognitive impairment after discharge.2 With these and other concerns in mind, methods to reduce critical care expenditures and ICU LOS—without negatively impacting patients—are of significant interest.3
One health system that is leading the way in critical care improvements is Allina Health, one of the foremost health systems in the Midwest. The largest of Allina Health’s three cardiac centers, the Minneapolis Heart Institute (MHI), created the first comprehensive CV emergency center at Abbott Northwestern Hospital (Abbott), one of the twelve hospitals within Allina Health. Providing emergency CV care to patients in the upper Midwest, the center is capable of immediately triaging and treating all forms of CV emergencies, while established protocols identify which patients need to be transferred to Abbott, and which can remain in their communities. This study describes how Allina Health improved CV services even more by increasing ICU bed availability without adding more staff or space.
KEEPING UP WITH DEMAND FOR EMERGENCY CARDIOVASCULAR CARE
Due to a high volume of patients, Abbott experienced intermittent shortages in ICU beds and medical staff. Although these shortages are common to so many hospitals, they pose real barriers to effectively and efficiently administering critical CV care. Patient flow becomes difficult to predict, with too much variation in patient placement processes. Patients and their families experience undue stress when patients are asked to move to a different unit, even if they have only just been admitted to an ICU room. Meanwhile, valuable staff time is essentially wasted on determining and documenting all of these movements.
Most seriously, patients sent to the ICU for only one night often don’t get the rest that is so important to healing. Even patients who are admitted to the ICU for a single night are vulnerable to experiencing ICU-associated complications, from the aforementioned delirium to delayed mobility. They’re also exposed to complications associated with increased use of intravenous medications for pain control. For some patients, admission to the ICU increased the complications experienced by the patient and contributed to a longer than desired LOS.
Abbott was motivated to evaluate its own patient placement processes, with the dual objectives of assuring ICU care for the most critically ill CV patients, while reducing ICU LOS—or avoiding the ICU altogether—for patients who would do better in another unit. In essence, Abbott sought a solution that would provide patients with the right care, in the right care setting, at the right cost.
AN ICU AVOIDANCE SOLUTION FOR STEMI, TAVR, AND CEA
Armed with expert knowledge regarding the care needs of CV patients, cardiac care leaders at the health system embarked on a multiyear journey to decrease ICU days, employing ICU avoidance strategies for select groups of CV patients. Having had previous success with use of decision support and analytics to facilitate risk assessment and changes in clinical practice, a similar plan was implemented for ICU avoidance.
Specifically, leadership planned to integrate evidence-based guidelines (where they existed) and risk assessments into decision support tools to guide patient placement decisions. To that end, leadership elected to leverage analytics based on information aggregated by the health system’s EDW from Health Catalyst. With a robust analytics platform in place, cardiac teams would be able to monitor important performance metrics of patients who initially avoided the ICU. These metrics included unplanned readmission rates, LOS, and cost of care.
Focusing on one group of patients at a time, leadership elected to first work on ICU avoidance for ST elevated myocardial infarction (STEMI); then move on to TAVR; and finally to elective carotid endarterectomy (CEA).
ICU Avoidance After a Severe Heart Attack
Percutaneous coronary intervention (PCI) is a non-surgical technique for treating obstructive coronary artery disease, including STEMI, unstable angina, and multi-vessel coronary artery disease. The technique is performed electively (unstable angina) and also more emergently (STEMI).
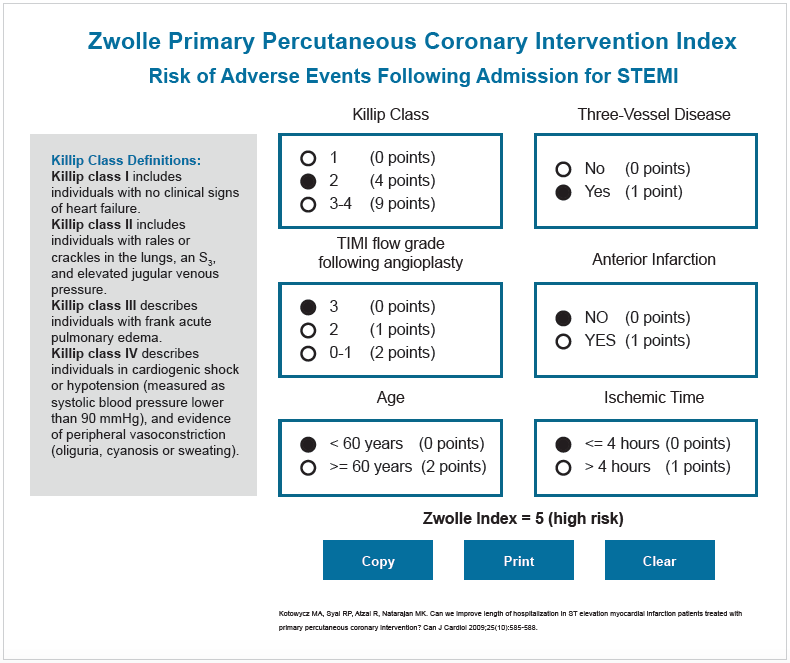
In the latter scenario, patients have historically been placed in the ICU post-intervention, even though not all needed to be. Cardiac care leaders were interested in learning if the Zwolle PCI Risk Index, a validated scoring tool for PCI, would be an effective way to determine which patients could safely avoid the ICU. The Zwolle scoring system generates a risk score between zero and 16. Patients with a score of three and under are deemed low risk, and have their heart rate and rhythm monitored for a short time after a PCI procedure. If no problems are detected, these patients can be safely discharged home after 48 hours. Patients with a score of at least four, however, are categorized as high risk and admitted to the ICU for more intensive monitoring and care.
Using data from the EDW, cardiac care leaders retrospectively applied the Zwolle PCI Risk Index to nearly 1,000 patients with severe heart attacks who had a PCI procedure at the hospital over a three-year period. The Zwolle classified 44 percent of these patients at high risk, and 56 percent as low risk. Statistically significant differences between the high risk and low risk groups were identified. No low risk patients had died in the hospital, while in-hospital mortality for high risk patients was 12 percent. Low risk patients also had far fewer complications.4
Confident that the Zwolle could accurately predict risk, the hospital prepared to select a non-ICU unit where low risk PCI patients could be placed. Elective PCI patients were admitted to the interventional telemetry unit post procedure. As the nurses on this unit were already comfortable providing care to post PCI patients, this unit was selected as the unit low-risk PCI STEMI patients would be placed as well. Of course, these patients differ from other PCI patients in that they have had a heart attack. Heart damage may have occurred that puts them at risk for future heart failure. Some patients experience grief, shock, or denial regarding their heart attack. The telemetry nurses understood these patients needed more assistance—emotionally and physically—and were prepared to provide it.
MHI at Abbott ultimately developed a real-time decision-support tool based upon the Zwolle and made it available at all PCI centers (see Figure 1). After clinicians were trained on the tool it was deployed to the desktop of all of the work stations in the catheterization lab, with no log-in or special permissions required since no patient information is stored in the application. The clinician makes selections for six elements that constitute the risk score, quickly identifying if the patient is low or high risk, and thus, which unit the patient should be assigned to.
PCI STEMI patients at low risk now avoid the intensive care unit entirely.
ICU Avoidance After Major Heart Surgery
CV care has evolved substantially over the last 15 years. Previously, for example, heart valve repair required open heart surgery via a sternotomy, a procedure in which the chest is surgically separated and opened. Post-op, patients of such invasive surgery were then transferred to the ICU. Patients who were not candidates for the surgery had no other treatment options. Today, the MHI heart team at Abbott performs transcatheter aortic valve replacement (TAVR), a procedure that replaces damaged valves through very small openings that leave all the chest bones in place.
After observing the effectiveness of ICU avoidance for STEMI patients, an interventional cardiologist requested ICU avoidance for transfemoral (TF) TAVR patients. Because TAVR is major heart surgery, this sparked considerable conversation about the appropriate care setting. With a goal of improving the patient experience and shortening LOS, Abbott elected to change the care model for these patients.
Previously, patients would go directly from the procedure to the ICU for recovery, usually for one night before transferring to a telemetry unit. The new care model bypassed the ICU altogether. Instead, patients moved from the procedure room to the post-anesthesia care unit for recovery, then to the telemetry unit after meeting certain recovery standards. In this unit, nursing staff were already accustomed to taking care of CV patients post-angiography and electrophysiology.
With confidence that the nurses had the foundational skills required, leadership prepared to communicate the change and assure nurses were adequately prepared and had the tools to support them in providing care to patients post TF TAVR. Education, provided by physicians and nurse educators in a variety of settings, was designed to build upon existing knowledge and patient care skills. The education focused on valve disease, with an emphasis on signs and management of complications post TF TAVR. Revised physician order sets and nursing guidelines were also made available to the telemetry unit.
Patients post-TF TAVR are now able to avoid the ICU. In an inspiring example, an elderly female patient was one of the first women in history trained to fly American military aircraft during World War II. While her valve disease would have ultimately contributed to her demise, her age and health condition made her ineligible for traditional open heart surgery. This veteran received TAVR, avoided the ICU post-op, and was discharged a mere three days after major heart surgery. Best of all, she returned to a more active lifestyle than she had prior to surgery.
ICU Avoidance for Elective Carotid Endarterectomy
Carotid Endarterectomy (CEA) is a surgical procedure to open or clean the carotid artery to prevent stroke. While the rate of complications for CEA is low, intense monitoring of neurologic and hemodynamic status are required to achieve these low rates, and the patient’s blood pressure must be tightly controlled. These factors have historically placed CEA patients in the ICU post-op. Leadership had explored ICU avoidance for these patients in the past, and following several periods of time when ICU beds and staff were short, revisited the idea in depth.
First, leaders used the EDW, an analytics application, and a vascular database to gain insight into CEA LOS. They discovered that postop CEA patients often went to the ICU for one night or just a few hours. Some patients were even discharged home from the ICU, suggesting overutilization of limited ICU resources. Following these discoveries, the hospital established a baseline measure for stroke rate, a key performance measure that would need to be maintained. Any change in patient location would need to result in continued high performance. On that note, leaders selected the vascular unit as the appropriate location for select post-op CEA patients. Nurses in this unit already provided care to a variety of vascular patients, including post-op CEA patients transferred out of the ICU.
To assist in appropriate patient placement decisions, the vascular surgeons developed a pre-op risk assessment and decision support tool. The decision support tool was validated by the registered nurses (RNs), and is completed by the vascular surgeon when the patient is scheduled for surgery. Importantly, this communicates the surgeon’s intention to have the patient avoid the ICU.
Vascular surgeons and RNs on the unit determined what safe care on the vascular unit would look like. Mandatory education on these best practices was delivered in person or available via recorded content.Potential revisions to the staffing model were drafted, as patients would need intense monitoring their first six hours in the unit. Here a cost analysis was also conducted, although leaders were aware that increases in staff hours might affect or negate any substantial cost savings. However, patient safety was the driving priority.
With the unit and care team providers ready to provide care, CEA patients began avoiding the ICU, moving immediately to the vascular unit following recovery in the PACU. Substantial support wasprovided to the RNs during the first two months of the change, which was essential for success. Evaluation data was collected at the unit level, enabling unit staff to share lessons learned and improve care processes even more.
Safety monitoring also took place in a similar vein as it did with the other patient groups. Using an analytics application based on data from the EDW, leaders monitored performance metrics such as stroke rate, ICU readmission rate, LOS, and cost. Case reviews were also regularly conducted for continued learning and development.
RESULTS
Allina Health’s ICU avoidance strategy is clearly providing better care for the health system’s cardiac patients at a lower cost. By avoiding ICU admissions for STEMI, elective CEA, and TAVR patients, Allina Health increased the availability of ICU care for those patients who need it the most—while decreasing the risk of serious complications such as ICU-induced delirium.
- 636 additional ICU days made available for more critically ill patients by employing ICU avoidance strategies.
- Proved that care of STEMI, TF TAVR, and CEA patients outside the ICU is safe and effective, with no increases in ICU readmissions rate and adverse events rate. For CEA in particular, there has not been a single incidence of stroke post-op, demonstrating that the RNs on the vascular unit are capable of appropriately monitoring the patients and managing changes in blood pressure.
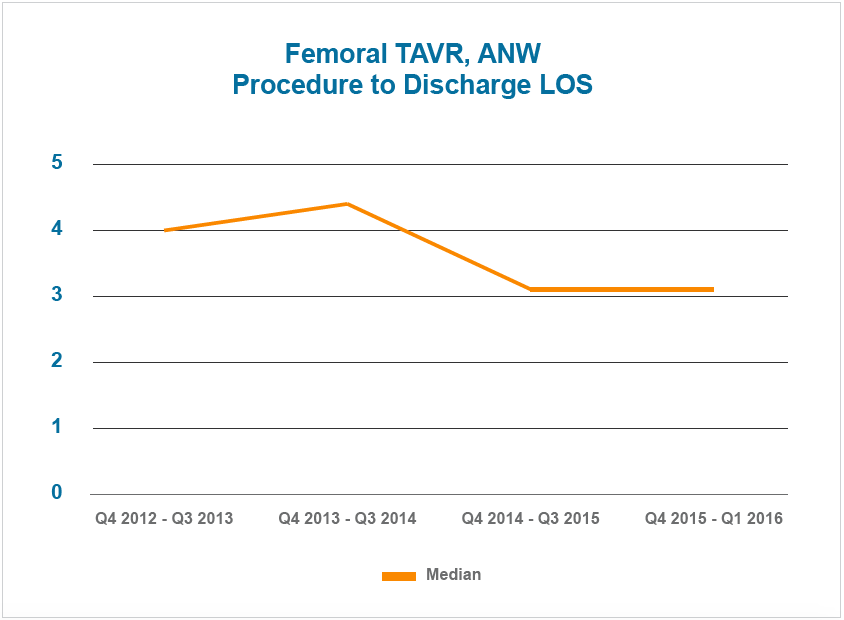
- One-day decrease in TF TAVR LOS (see Figure 2). Patients who avoid the ICU are mobilized sooner, and started on oral pain control faster than they would have traditionally been. This contributes to increased patient readiness for discharge, decreasing overall LOS.
- $589,342 cumulative cost savings achieved by reducing ICU days for STEMI ($332,223), TF TAVR ($178,525), and elective CEA ($78,594).
“Use of a decision-support enabled risk assessment tool in the cath lab is a really great example of how evidence-based, and technology-enabled, decision-support tools can help standardize practice.”
– Pam Rush, RN, MS
Cardiovascular Clinical Service
Line Program Director
WHAT’S NEXT
With the right analytics tools at hand, Allina Health plans to increase the number of patients who successfully avoid the ICU. In the long term, the health system will continue to evaluate different care models, always working to assure that the right care is provided, in the right care setting, at the right cost.
REFERENCES
- Halpern, N.A. & Pastores, S.M. (2010, January). Critical care medicine in the United States 2000-2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med., 38(1):65-71. doi: 10.1097/CCM.0b013e3181b090d0
- Salluh, J.F., Wang, H., Schneider, E.B., Nagaraja, N., Yenokyan, G., Damluji, A., Serafim, R.B. & Stevens, R.D. (2015) Outcome of delirium in critically ill patients: systematic review of meta-analysis. BMJ, 350:h2538.
- Vincent, J.L. & Rubenfeld, G.D. (2015, March 2) Does intermediate care improve patient outcomes or reduce costs? Crit Care., 19(1): 89. doi: 10.1186/s13054-015-0813-0
- Strauss, C. (2013, October 11). Shortening hospital stays for lower-risk patients after a severe heart attack. Harvard Business Review.
ABOUT HEALTH CATALYST
Health Catalyst is a mission-driven data warehousing, analytics, and outcomes improvement company that helps healthcare organizations of all sizes perform the clinical, financial, and operational reporting and analysis needed for population health and accountable care. Our proven enterprise data warehouse (EDW) and analytics platform helps improve quality, add efficiency and lower costs in support of more than 50 million patients for organizations ranging from the largest US health system to forward-thinking physician practices.
For more information, visit www.healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.