Optimizing Sepsis Care Improves Early Recognition and Outcomes

- 14.1 percent relative reduction in mortality for patients with severe sepsis and septic shock.
- 24.9 percent relative difference in mortality for patients that received the evidence-based protocols compared to those who did not—the evidence-based protocols substantially reduce mortality.
- 6.4 percent relative reduction in emergency department (ED) length of stay (LOS) for patients with severe sepsis and septic shock.
- Four percent relative reduction in ICU LOS for patients with severe sepsis and septic shock admitted from the ED.
Early identification of sepsis is challenging, as the patient’s physical response to this overwhelming infection presents as a syndrome of non-specific symptoms, delaying recognition, diagnosis, and treatment, which increases mortality rates.
Mission Health, North Carolina’s sixth largest health system, had implemented evidence-based sepsis care bundles; however, processes for identifying patients with sepsis and initiation of care was fragmented and varied widely across the system, negatively impacting sepsis outcomes.
Using a comprehensive data-driven approach to facilitate early sepsis identification and standardize the treatment of sepsis, including the addition of evidence-based alerts, Mission has gained insight into sepsis performance to drive improvement.
SEPSIS: A POTENTIALLY FATAL CONDITION
In the U.S., over 1.5 million people will get sepsis annually, a condition that carries a high risk of death. Approximately one in three deaths of people in the hospital are a result of sepsis, causing nearly 250,000 people to die each year.1
Early identification of sepsis is challenging, as the patient’s physical response to sepsis, an overwhelming infection, presents as a syndrome of non-specific symptoms, leading to delayed recognition, diagnosis, and treatment, which increases mortality rates.2 Evidence-based assessment tools help identify patients with sepsis sooner, and care bundles help facilitate early treatment, particularly within the first hour of detecting sepsis, leading to reduced mortality rates.3
Previously, the gold standard for diagnosing sepsis was systemic inflammatory response syndrome (SIRS). In 2016, the Society of Critical Care Medicine and the European Society of Intensive Care Medicine published a new clinical definition of sepsis based upon organ dysfunction, with recommendations to use a sequential organ failure (SOFA) score to identify patients with sepsis.4
Mission, based in Asheville, North Carolina, is the state’s sixth largest health system with six hospitals, numerous outpatient and surgery centers, and is the region’s only dedicated Level II trauma center. Mission’s BIG(GER) Aim drives its daily work to improve outcomes by helping every person to achieve their desired outcome, first without harm, also without waste and always with an exceptional experience for each person, family, and team member. Reducing the sepsis-related LOS and mortality rates became a priority for the organization.
DELAYED SEPSIS IDENTIFICATION
Mission had previously implemented evidence-based sepsis care bundles; however, processes for identifying patients with sepsis and initiation of care were fragmented and varied widely across the system, negatively impacting patient outcomes. Data informing sepsis improvement performance was difficult to obtain and relied largely on manual chart audits, making it challenging to develop improvement goals, monitor efforts, and limited the ability to provide meaningful feedback regarding sepsis outcomes.
Early alerts within the EMR used SIRS criteria and non-specific signs and symptoms to determine if the patient had a source of infection or organ dysfunction, leading to frequent false positives and alert fatigue, making early identification of sepsis difficult.
To overcome these obstacles, Mission piloted a paper process to augment the EMR alerts systems, however, having two workflows for the nursing staff further delayed sepsis identification. The health system had developed evidence-based orders sets, implementing three-hour and six-hour bundle components, but did not have a comprehensive implementation communication plan, leading to lacking engagement in the improvement efforts.
Mission needed to look at alternative approaches for identifying sepsis in order to reduce LOS and mortality rates of patients with severe sepsis.
ACCESS TO ANALYTICS HELPS OPTIMIZE SEPSIS CARE
Mission used a comprehensive data-driven approach to facilitate early sepsis identification and to standardize the treatment of sepsis. To facilitate change, the health system convened a multidisciplinary sepsis improvement committee charged with standardizing sepsis-related care across the organization. Committee membership includes emergency physicians, hospitalists, critical care physicians, nursing leadership, pharmacists, lab staff, performance improvement specialists, and data analysts.
To gain insight into sepsis performance to drive improvement, Mission leveraged the Health Catalyst® Data Operating System (DOS™) Platform, implementing the Sepsis Prevention analytics application.
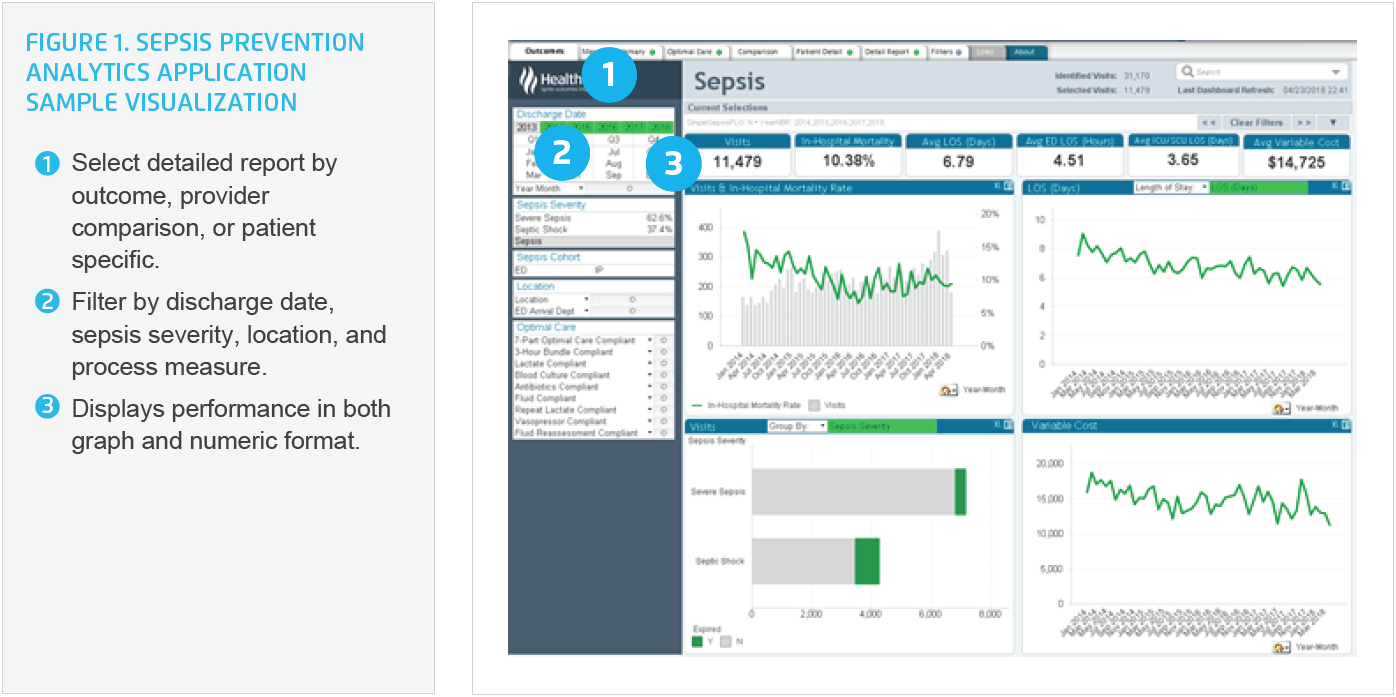
The analytics application is designed for clinicians, medical directors, operational directors, and clinical program guidance teams in the emergency, intensive care, and inpatient units. This tool provides near real-time actionable data to help improve early recognition of sepsis, rapid intervention for severe sepsis, and prompt therapy for septic shock to reduce mortality and LOS (see Figure 1).
Using the advanced application, Mission reviewed historical data to understand the sepsis population characteristics, finding that over 70 percent of the patients with severe sepsis were admitted from the ED, making the ED the priority for initial improvement efforts.
The committee first implemented its improvement initiative in Mission’s largest ED, developing a plan with two primary aims: identify severely septic patients and provide standardized, evidence-based care to patients with severe sepsis.
Identifying severely septic patients
The committee developed a tiered approach to early identification of sepsis, distinguishing three key factors needed to improve:
- Modifying the SIRS screening tool.
- Incorporating the evaluation of organ dysfunction as part of the sepsis screening process.
- Developing a “code sepsis” team activation process to expedite care in the ED.
Alerts in the EMR were reviewed and compared to evidence-based criteria, refining the original SIRs vital sign inclusion standards. For example, the heart rate criterion was modified to trigger an alert for sepsis if the heart rate is greater than 120.
The committee also designed a sensitive and specific screening tool using the revised vital sign criteria and the determination of the possible source of infection, decreasing the volume of false positives and alert fatigue, and increasing the percentage of patients who are accurately identified with severe sepsis. This revised screening tool was built within the EMR and integrated into the registered nurse (RN) workflow, facilitating universal rapid screening for sepsis upon patient arrival.
When screening inclusion criteria are met, a sepsis alert is automatically triggered, activating the RN to obtain labs including blood cultures, lactate, complete blood count, and metabolic panels. The provider also receives the alert notification informing them that the patient potentially has severe sepsis. In conjunction with reviewing lab results, the provider evaluates organ dysfunction using the quick sequential organ failure assessment (qSOFA). The qSOFA includes one point for:
- Systolic blood pressure ≤100 mmHg.
- Respiratory rate ≥22 breaths per minute.
- Altered mentation measured using the Glasgow coma scale score <15.
If the patient scores two or greater, the provider activates a “code sepsis.” This code brings a response team, including an ED physician, RN, respiratory therapist, radiology staff, lab personnel, and pharmacist to the patient bedside to expedite care.
Standardizing sepsis care reduces variation
The committee developed a sepsis power plan, a set of protocols and order sets accessed by one click within the EMR, to reduce care variation. The evidence-based bundled care interventions initiate nursing, lab, and pharmacy workflows, facilitating early treatment interventions.
The committee relies on data within the analytics application to monitor process measures associated with the order sets and protocols to identify any barriers in delivering rapid treatment. Process measures include:
- Positive response to the screening tool and sepsis alert defines “time zero” of sepsis identification.
- The time from time zero to the time the order for lactate is placed.
- Length of time between time zero and the time of antibiotic administration. The goal is less than one hour.
- The duration between time zero and the administration of an IV fluid bolus for patients in septic shock, defined by lactate level greater than four.
- Use of the complete order sets and protocols for patients with sepsis.
Having the screening tool and evidence-based order sets and protocols in place, Mission developed and delivered comprehensive education to all clinicians who care for patients with sepsis, including providers and nursing staff. Ongoing education is provided as new team members join, ensuring standard use of the evidence-based care processes.
Mission further optimizes sepsis care by engaging bedside clinicians in role-specific components of the clinical care. For example, the delivery of antibiotic within one-hour of arrival requires different workflows for the providers ordering the antibiotics, the pharmacist verifying medication order, and the RN administering the antibiotics.
The sepsis committee and leaders widely use the near real-time, drill down data available within the analytics application to provide meaningful performance feedback to all staff involved in sepsis care.
- The ED physician champion uses the analytics application to develop monthly case studies outlining bundle component omissions and shares them with clinicians through email newsletters and monthly meetings. The timeliness of these specific use cases allows providers to reflect on their practice and immediately identify opportunities for improvement.
- Nursing leaders review the analytics daily, providing timely feedback to nursing staff, celebrating successes, and identifying areas where there are barriers to timely treatment. This helps foster a culture of continuous improvement.
- Quality improvement leaders use the data within the analytics application in developing their reports and monitoring regulatory compliance. Routine use of the technology supports early identification of any areas that may be falling behind expected outcomes, further enabling a culture of continuous improvement.
Through frequent use of the application, the committee determined that repeat lactates for patients who had initial lactate greater than two were being missed. By engaging clinicians in the improvement efforts, Mission designed an automated process to order repeat lactate lab draws given certain clinical criteria. This step improves compliance with this measure and provides clinicians timely access to diagnostic data needed for patient treatment.
Mission has spread its standard sepsis care across the system in both the ED and inpatient care areas, further spreading early identification and treatment of sepsis, improving patient outcomes.
RESULTS
Using this comprehensive approach for early recognition and treatment of sepsis, Mission has achieved substantial improvements in sepsis outcomes, including:
- 14.1 percent relative reduction in mortality for patients with severe sepsis and septic shock.
- 24.9 percent relative difference in mortality for patients that received the evidence-based protocols compared to those who did not—the evidence-based protocols substantially reduce mortality.
- 6.4 percent relative reduction in ED LOS for patients with severe sepsis and septic shock.
- Four percent relative reduction in ICU LOS for patients with severe sepsis and septic shock admitted from the ED.
“It is important to be vigilant with reviewing the data, providing ongoing monitoring and feedback. This is particularly important when new members join the healthcare team, or sepsis definitions change. Staying informed helps ensure we avoid care variation and decreases in patient outcomes.”
– Jeanie Bollinger
Clinical Nurse Specialist
Acute Medicine, Mission Health
WHAT’S NEXT
Mission will continue to use this proven plan to improve sepsis outcomes and enhance care for patients with sepsis. The health system is setting the groundwork to move the early identification screening tools to the outpatient setting, including urgent care centers and physician offices.
REFERENCES
- Centers for Disease Control and Prevention. (2018). Sepsis – data & reports.
- Nagalingam, K. (2017). Ensuring early recognition and treatment of sepsis and septic shock. Nursing Times, 113:2, 35-37.
- Surviving Sepsis Campaign. (n.d.). SSC hour-1 bundle.
- Fujishima, S. (2016). Organ dysfunction as a new standard for defining sepsis. Inflammation and Regeneration, 36, 24.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.