Improving Patient Safety: Machine Learning Targets an Urgent Concern
Patient harm is a persistent and urgent healthcare concern that directly impacts the patient experience and overall outcomes. According to recent estimates, one in three hospitalized patients experiences preventable harm, and over 400,000 individuals per year die from these injuries. As the third-leading cause of death, preventable harm costs health systems more than $1 billion annually.
As health systems seek ways to improve patient safety, many organizations are looking to patient harm risk assessment tools that leverage machine learning. This article describes how machine learning powers better risk prediction tools, with the eventual goal of helping clinicians identify safety concerns before the patient harm occurs.
Better Risk Prediction Tools Consider Whole-Patient Risk
Previous risk prediction models were limited because they were developed using populations different from the populations for which the tools were being used. Another downside to these out-of-the-box models (such LACE, which predicts readmissions) is that they were often trained on data that was 15 to 20 years old. These generalized tools were also siloed in stand-alone prediction systems; for example, rather than an all-cause harm view of potential safety events, a risk assessment tool looked at only one event (e.g., hospital readmissions for patients with chronic obstructive pulmonary disease, or COPD).
Patients tend to be at risk for a variety of negative outcomes, so with a siloed risk assessment approach, clinicians miss opportunities to manage or prevent harm. The patient safety community has devised a whole patient measure of safety to address siloing in measuring patient harm. The same concept needs to be applied to risk prevention. A better, machine learning-powered patient safety tool uses health system data to assess whole-patient risk, giving clinicians a comprehensive view of patients who are at risk for a safety event, including identifying the particular event(s), as well as modifiable risk factors.
Machine Learning Enables Timely Risk Identification
This new generation of machine learning-based patient safety tools will close the loop between information and action, as the software not only forecasts the likelihood of harm, but also the most important clinical actions to lower that patient’s risk, helping the clinician make an informed intervention decision. Clinicians will be able to predict harm before it occurs, know who in their patient population is at risk, understand which of the patient’s modifiable risk factors need to change, and be able to make timely interventions.
Improving Patient Safety with Five Must-Have Machine Learning Capabilities
To successfully reduce rates of patient harm, today’s patient safety risk assessment tools must have five core capabilities:
- Identifies risk: provides concurrent daily surveillance for all-cause harm events using literature-based triggers to show how many patients in a health system population are at risk for safety events (e.g., CLABSI).
- Stratifies patients at risk: places at-risk patients into risk categories (e.g., high, medium, and low risk).
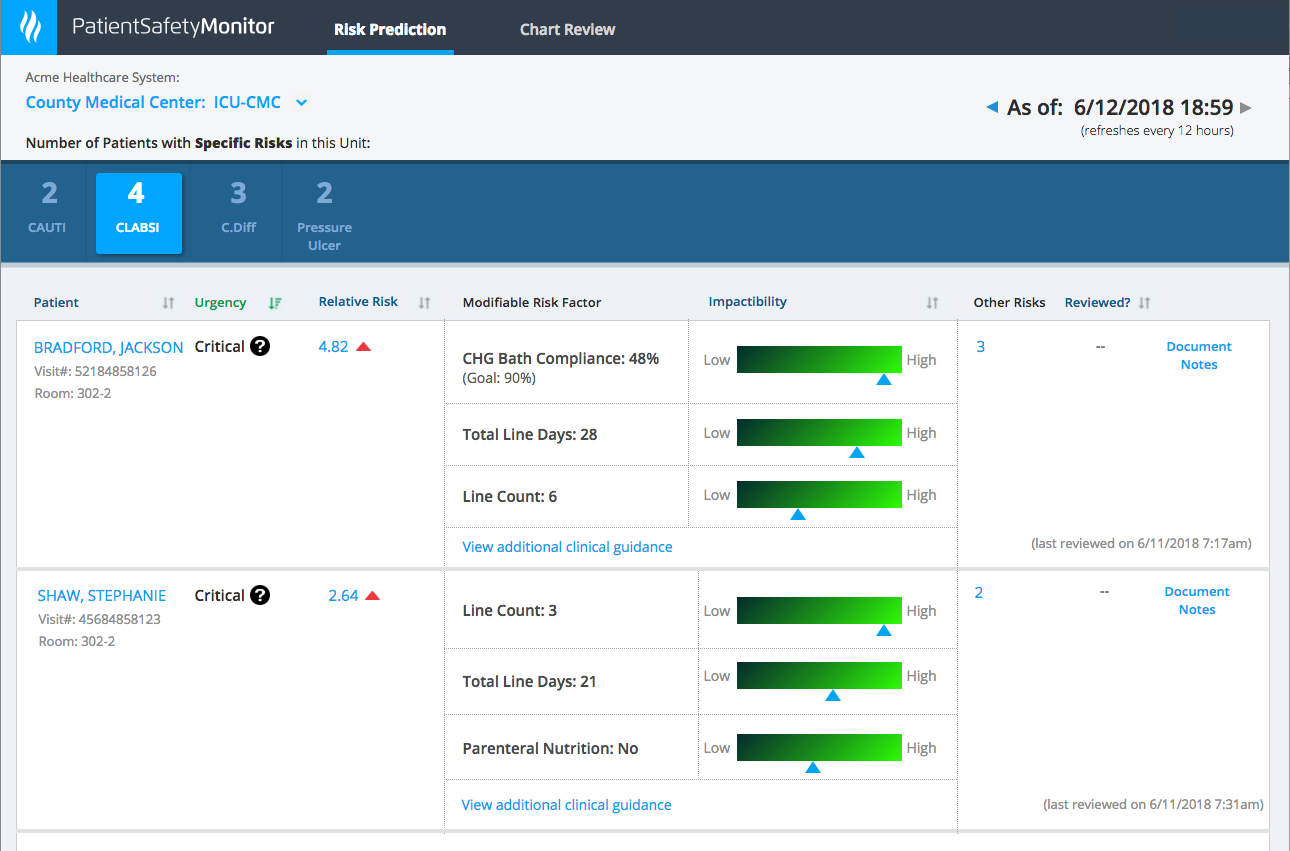
- Shows modifiable risk factors: by understanding a patient’s modifiable risk factors and the degree to which they can be impacted, clinicians know where to intervene to prevent harm. Modifiable risk factors for a condition such as CLABSI include line days, number of lines, bathing rates, and compliance with bundles (interventions that, when implemented as a group, have a greater effect than individual interventions alone).
- Shows impactability (Figure 1): offers clinical decision support that helps clinicians identify high-risk patients and prioritize treatment by patients who are most impactable (most likely to benefit from preventive care).
- Makes risk prediction accessible: integrates risk prediction into workflow tools for immediate access.
The major differentiator between the new generation of machine learning safety surveillance and the retrospective tools they’re replacing is that the machine learning tools use data from that same health system to not only understand the risk factors leading to harm, but also to identify which patients currently receiving care are being harmed or about to be harmed. Machine learning capabilities help organizations get upstream of the risk before a patient is harmed or at risk of harm.
Eventually, predictive patient safety tools will advance the way organizations mitigate patient harm by recommending interventions for modifiable risk factors and documenting those interventions. The next goal is to integrate with cost management tools to attribute cost and recommend data-driven, cost effective interventions.
Machine Learning for Patient Safety: A Much-Needed Solution
With the current, unacceptably high rates of preventable patient harm occurring in health systems, improving patient safety is a critical healthcare mission. Machine learning will drive the solution by enabling safety surveillance tools that use health system data to identify patients at risk, identify patients’ modifiable risk factors and impactability, and, eventually, recommend the most cost-effective interventions.
Healthcare’s best chance of improving patient safety and outcomes lies in predicting harm and taking action to prevent it. As Don Berwick, MD, MPP, president emeritus and senior fellow at the IHI, explained in his keynote address at the 2017 National Patient Safety Foundation Patient Safety Congress, healthcare has a lot of work to do to improve patient safety. “There’s an illusion that we’ve worked on safety,” Berwick said, and added that healthcare hasn’t developed real insight into patient harm and ways to prevent it. With a comprehensive, concurrent data-driven approach to patient harm, machine learning promises to transform patient safety from illusion to reality.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
- How to Use Data to Improve Patient Safety
- Patient Flight Path Analytics: From Airline Operations to Healthcare Outcomes
- Sepsis Mortality and Length of Stay: One Hospital System’s Story
PowerPoint Slides
Would you like to use or share these concepts? Download this presentation highlighting the key main points.
Click Here to Download the Slides
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

