Understanding Population Health Management: A Diabetes Example
The World Health Organization reports that nearly 1.5 million people die from diabetes annually. In addition to the devastating mortality rate, health experts estimate on a global scale the cost of diabetes will reach $2.1 trillion by 2030.
Given its prevalence and economic impact, diabetes is representative of the chronic health conditions at the root of global healthcare challenges, highlighting the need for population health management. With an effective approach to managing the health of populations, providers and healthcare organizations can improve the quality and reduce the cost of diabetes care worldwide.
Managing Diabetes with Healthcare Data
One challenge of addressing a chronic health condition, such as diabetes, is that symptoms often aren’t apparent until significant damage has occurred. For example, an individual with newly-diagnosed Type 2 diabetes may have no signs indicating a problem, though test results would prove otherwise. Such unreliable symptoms make a more trustworthy approach—one that leverages healthcare data—critical in diabetes management.
For example, glucose control and therefore glucose data are key to minimizing the risk of many complications stemming from Type 1 or Type 2 diabetes. The higher a patient’s hemoglobin A1c level, the poorer their blood sugar control and the higher their risk of complications. In fact, studies have shown that every percentage point drop in A1c blood test results can reduce the risk of eye, kidney, and nerve disease complications by as much as 40 percent. As a result, patients and clinicians need continual access to timely data to maintain target glucose levels.
Management by Measurement: A Personal Anecdote on Managing Diabetes via Data
On a personal note, I’m very conscious of the need to manage my own Type 2 diabetes by monitoring data and trends. Historically, my A1c had been well-controlled. Several years ago, however, it was measured at 7.8. I felt fine at the time, but my A1c was clearly trending in the wrong direction, which put me at a higher risk of complications. In 2014 I set a personal goal of getting into the lowest-risk category, by consistently having my A1c readings below 7.
My goal took discipline and effort. I was determined to lose weight and walked least 10,000 steps per day—the equivalent of walking about five miles. I also closely monitored my intake of carbohydrates, which is a key intervention for any diabetic. In less than a year, I lost 18 pounds and decreased my A1c to 7.4.
Jumping forward to 2021, my battle with diabetes continues. My A1c has fluctuated up and down but has averaged around 7.2. In 2020, I focused more on biking and decreased my weight by another 12 pounds. The COVID-19 pandemic has given me more time to focus on intense cycling, and I finally reached my goal of an A1c of 5.9 (Figure 1).
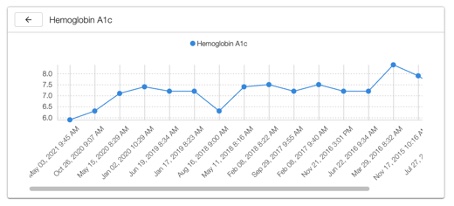
Figure 1: The author reached an A1c of 5.9 in 2021.
It has been a long journey, but I’m now in the lowest risk group, with my A1c only slightly above normal (a non-diabetic upper limit is 5.7). Additionally, my primary care provider recommended I cut my dose of glimepiride (an oral hypoglycemic agent) in half. This marks the first time since my diagnosis 12 years ago that I have decreased my diabetes medications, and it feels great! I am due for another A1c check in fall 2021 and looking forward to seeing my progress so I can learn and adjust diabetes management to reduce my risk of complications and mortality.
I tell this story to make the following point: When managing chronic conditions like diabetes, one can only manage what they can measure. Engaging patients in active management of their disease metrics is essential to managing any chronic disease. Regularly scheduled measurements coupled with care coordination and appropriate intervention is the best approach.
Population Health Management: Managing Diabetes Populations
Scaled to a population level, the personal anecdote above demonstrates
how successful population health management starts with measuring and accurately identifying a population with diabetes and monitoring how the disease trends. These tasks have been difficult in the past, but advanced analytics tools and healthcare data platforms, such as the Health Catalyst Data Operating System (DOS™), are making population health monitoring more accessible.
By aggregating data from multiple sources, a data platform provides the foundation for sophisticated diabetes population management, such as the following:
- Create and maintain a robust diabetes registry.
- Use diagnosis codes supplemented by clinical information to continue to define and refine the diabetes population.
- Identify patients who aren’t up to date on tests, including A1c, fasting lipids, blood pressure, microalbumin, and more.
- Establish benchmarks and compare those to state and national benchmarks.
- Identify diabetic patients with the highest risk of high cholesterol, hypertension, or heart disease.
- Monitor and report on key indicators for diabetes complications.
- Rank patients by number of care deficits to prioritize outreach efforts.
- Measure the success of diabetes management interventions.
- Discover variations in diabetes care across an organization.
- Reduce waste.
- Understand exactly how diabetes care affects an organization’s costs.
Creating Better Diabetes Outcomes
The best opportunity for better outcomes for diabetes patients—and those with other chronic diseases—lies in effectively leveraging data. A data platform enables organizations to identify high risk patients with diabetes and those with treatment or screening gaps. Organizations can then prioritize and target interventions to those specific patient groups. Good data management and patient access also enable each individual to better manage their own diabetes by the numbers.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

