Activity-Based Costing in Healthcare During COVID-19: Meeting Four Critical Needs
While healthcare’s move from a fee-for-service to a value-based care (VBC) model has been taking hold over the past decade, the financial strains and uncertainty of COVID-19 have placed increasing urgency on cost management. As health systems emerge from the acute phases of the pandemic, financial recovery rests on understanding the true cost of their services.
Critical cost insights in the post-COVID era will include the following:
- Reliable understanding of an organization’s services’ impacts on patient outcomes.
- The tools to negotiate payer contracts as well as understand and adapt to the impact of new and changing pricing schemes.
- Disparate data sources including claims, clinical, cost, and geospatial data to make intelligent strategic decisions (e.g., make versus buy, capital planning, mergers and acquisitions, etc.).
An effective costing solution is a critical asset in the newer payment landscape, in which increasing capitation will place more importance on the strategic use of resources to deliver quality care. Yet, building the right healthcare costing tool comes with significant challenges that only advanced and expert-driven technology can resolve. Organizations can best prepare for the inevitable changes under VBC with an activity-based costing (ABC) solution that delivers detailed and actionable cost data across the analytics environment, supporting service-line reporting, contract modeling, strategic decision making, and clinical process improvement.
Meeting the Top Challenges of Building an Effective Healthcare Costing Solution
Healthcare financial experts with frontline experience (such as building homegrown ABC systems), who understand the challenges, politics, and complexity of costing, point to three critical solution competencies:
Data Management and Scalability
Healthcare organizations need a data management strategy that involves communication across source systems, eliminating silos, and integrating cost data with organizational analytics. As the standard way to analyze cost data, most health systems will either have a traditional costing system or rely on an analyst using Excel to compile general ledger (GL) costs and combine them with charge code data. These approaches can be a viable costing solution to—a point.
With limitations including manual entry, lack of granularity, and insufficient data capacity for today’s increasingly digitized healthcare industry (e.g., between hundreds of thousands to millions of rows of patient activities each month associated with cost) and the more robust criteria for ABC, old methods based on charge codes, with hundreds of analyst hours required, can’t meet today’s needs. In addition to taking excess time, traditional approaches provide the wrong answers to the wrong questions. Costing based on charge codes results in an “averages of averages” that doesn’t reflect the true consumption of costs. Data captured each day by modern EMRs enables measuring true consumption with metrics including staff time, nursing minutes, and detailed supply and drug utilization. Leveraging EMR data in costing, however, requires a robust new costing model to support the new way of thinking.
Data management technologies that emerged in 2012 through powerful cloud and computer technologies offered enhanced scalability, enabling health systems to apply ABC to their operations and lay the groundwork for next-generation costing systems. Since then, newer, more sophisticated systems, such as the Health Catalyst® CORUS® Suite, have the advanced capabilities to not only enable ABC but provide an easy interface to validate and govern the massive amount of colliding financial and clinical data. These former systems were based primarily on billing data (charge detail). They used the ratio of costs to charges (RCC) or relative-value units (RVU) methodologies (pure allocation methodologies based on broad assumptions) in the place of more detailed direct and indirect costs. In this way, an advanced costing system gets to the cost per activity and true patient profit-and-loss statement, providing the credibility that was missing from older costing systems.
With more credibility, clinical and operational team members and leaders will more likely accept the premise of the data. From a clinician perspective, data based solely on charges doesn’t appear relevant to their work or patients. Direct and indirect costs, cost per activity, and actual patient profit-and-loss statements, however, more effectively engage clinicians to make cost-effective practice changes, as they understand exactly how their choices impact the cost.
Credibility enables ABC to drive true change across an organization, furthering operational goals and outcomes improvement-related efforts to lower cost, become more efficient, and reorganize around service lines.
A next-generation costing system has the following advanced data management capabilities:
- Applies logic every month, ensuring all patients are costed: Older costing systems account for only inpatient cost and lack ambulatory data, excluding all facility users who aren’t admitted to a hospital. A newer system incorporates ambulatory data and ingests all the information from the patient journey—profit and loss for the whole stay—that influences cost (e.g., how long a patient is in one room).
- Can grow with an organization’s currently unknown costing needs over time: For example, just basing costing needs off of charge codes or simple operational data won’t suffice in the future when the industry looks for real-time locating systems (RTLS) data.
- Leverages a common platform for all data (e.g., a cloud-based platform such as the Health Catalyst® Data Operating System (DOS™): The first step in accurate costing is to have a data warehouse to bring in data from multiple different sources and a means of capturing information beyond the EHR (from the patient bedside to outpatient and virtual services, wearable sensors, etc.). Historic costing solutions have been limited to one or two data sets.
- Reconciles detailed costing output to monthly and yearly financial statements: Anchoring to a source of truth is essential for trusting and accepting the cost results.
- Positions organizations to measure and look for the most critical data for their work: Various technology captures a lot of data about each patient, but accurate costing only needs certain elements. Advanced costing sifts through massive data sets for those critical pieces of information, forcing organizations to identify the source of truth for each set of metrics and standardize around it. For example, developing calculations around room-in to room-out time in the operating room, total nursing, IT, and other staff time involves several vital tables from the EHR. Perhaps the imaging area uses a separate system for documentation that contains key information about contrast costs. Organizations want to use the best data about the services they provide when costing their business.
- Calls out inefficient areas in a health system (e.g., determining if one operating room is more efficient than another): Applying the same costing principles to different places in the organization performing similar tasks—down to cost per minute and cost per visit—highlights efficiency and opportunities for improvement in high cost/low throughput areas.
- Identifies data quality and documentation problems: These problems include process issues at the point of care; identifying them helps standardize workflows by addressing processes that aren’t up to organizational standards.
- Shows ongoing performance, eliminating the need for one-time cost analysis: For example, understanding the cost at an organization of a procedure is a historically time-intensive, manual process (due mainly to the time it takes an analyst to hunt and gather data). When organizations calculate performance data on an ongoing monthly basis, they don’t need to rely on manual analysis to calculate each procedure. The costing system perpetually generates data, so users only need to refresh the pivot table (a tool that extracts the significance from an extensive, detailed data set). They can count on the same methodology behind historical cost allocations applied to the most recent months of data for similar patient populations.
Ongoing Maintenance
One of the harder challenges of costing is maintaining a solution that combines many different data sources as they provide the translation. Location codes in one system for an operating room look completely different than a clinic location in another database, making mapping them to the associated GL cost center essential. Due to the challenge of storing voluminous detailed EMR data, older costing systems based on charges got around mapping by relying mainly on the detailed charge data from a billing perspective. Because an advanced costing system is more prone to data quality issues, given the size and scope of the input data, it has pre-built checks for the most common problems.
In general, the primary costing maintenance steps are as follows (Figure 1):
- Pre-cycle source data quality and validation checks (known as pre-checks).
- Executing or scheduling the cost engine to run.
- Reviewing and reconciling the resulting output compared to the GL.
A more straightforward maintenance process, with the right guardrails, makes it easier to create new costing intelligence at the grain necessary for it to be meaningful. Some people believe an advanced ABC system is more difficult or cumbersome to maintain than older solutions, which isn’t always the case. Older solutions require users to maintain RVUs by charge code or rely on charge amounts that do not reflect the true cost of providing care. Maintaining charge codes is no longer needed when calculations, such as time in room, are done procedurally by subtracting a room-out from room-in time field within a line of SQL code. The calculation is free of the bias possible in conversations about the often highly subjective relative value or relative cost between two charge codes.
An ABC solution, such as CORUS, has progressed to the point where one person can maintain the system in a few days each month and can regenerate years of historical data in a matter of hours. Older solutions—if they offer the service—would require months of effort from many team members to test and apply updated logic. The architecture of newer costing systems frees up analysts’ time from maintaining outdated methodologies and hunting for data to maintaining the translation between different data silos.
Adoption
Positioning a costing system for healthcare organization adoption is a critical area of strategy. Primarily, financial teams must present costing system output so clinical and financial leaders will accept the numbers. The strategy that helped develop the tool may not work as well for adoption, so financial teams need to think about how they approach leadership specifically.
A next-generation costing system strategy must aim for organizational buy-in during development, not only at the time of rollout. Users and key leaders are more likely to accept an end product when they’ve been consulted in its development. Costing systems developers must approach each party’s concern (e.g., clinical, IT, financial). CORUS, for example, can show these different perspectives and get the three groups on the same page, speaking the same language.
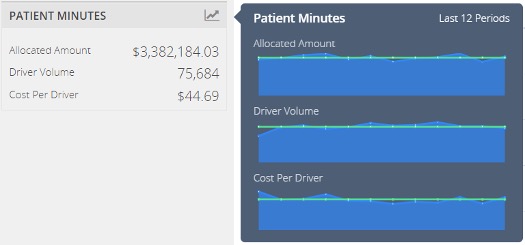
The example in Figure 2 for an operating room cost center shows the allocated dollar amount from the GL (agreed on by finance), the driver volume of 75,684 minutes as calculated from the EMR surgery module (code signed off on by IT/finance/clinical), and the cost per driver, which is applied to each patient in the costing period.
Widespread buy-in positions the costing system as the ultimate source of financial truth and enables different parties to sustain communication with each other, as clinical, IT, financial, and other departments don’t always naturally collaborate.
Healthcare Activity-Based Costing Drives Better Financial and Clinical Outcomes
By adopting a next-generation costing tool, organizations can leverage ABC to drive financial and clinical outcomes improvement like these success stories:
- Activity-based costing and clinical service lines team up to improve financial and clinical outcomes: When an academic medical center recognized the common denominator to addressing threats to sustainability was fully understanding and effectively managing costs, it leveraged an advanced costing solution to implement ABC. This initiative delivered detailed and actionable cost data across the analytics environment and supported service line reporting and clinical improvement, helping the organization drive cost savings and improve clinical outcomes. Initial improvements included $3 million cost savings.
- New generation activity-based costing accelerates timeliness of decision support: In healthcare, the timely delivery of patient-activity level cost metrics to clinical, financial, and operational leaders is critical. These insights allow the organization to respond to internal and external shifts and challenges to positively impact financial performance without negatively impacting patient care and experience. An academic medical center implemented an analytics-driven cost management system. It achieved a 50 percent reduction in the time needed to complete month-end close, allowing many months of data to now run simultaneously and providing a foundation for a new data-driven governance structure.
A Costing Solution for COVID-19-Era Healthcare Challenges and Beyond
As increasing digitization, the continuing shift to VBC, and new complexity amid COVID-19 promise to drive growth in and demand for health data, today’s healthcare organizations need a costing solution that can keep up with the data and meet associated challenges. With the right next-generation ABC tool, health systems can access the detailed data they need to address the challenges of lowering the cost of care, automating costing activities, and reducing administrative costs, particular as they face new financial strain associated with the pandemic. Finally, organizations can then pass those savings along to patients.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
- Health Systems Share COVID-19 Financial Recovery Strategies in First Client Huddle
- How Data Transforms the Hospital Command Center to Pandemic Proportions
- Restarting Ambulatory Care and Elective Procedures: Analytics Guide Safe, Pragmatic Decisions
- How UPMC and Health Catalyst Improve Outcomes Using Innovation in Activity-based Costing
- Activity-Based Costing: Healthcare’s Secret to Doing More with Less
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

